When a drug carries a black box warning, it’s the FDA’s loudest alarm. For antidepressants used in children and teens, that warning has been ringing since 2005 - and it’s changed how doctors prescribe, how parents decide, and how many young people get help. But here’s the uncomfortable truth: the warning may be saving lives in theory, while accidentally costing them in practice.
What the Black Box Warning Actually Says
The FDA’s black box warning on antidepressants for youth isn’t subtle. It’s bold, black-bordered text that appears on every prescription bottle and patient guide. It states clearly: "Antidepressants increase the risk of suicidal thinking and behavior (suicidality) in children and adolescents with major depressive disorder and other psychiatric disorders." This warning applies to all prescription antidepressants - SSRIs like fluoxetine (Prozac), sertraline (Zoloft), and escitalopram (Lexapro), as well as SNRIs like venlafaxine (Effexor). It doesn’t matter which one, how much, or how long. If it’s prescribed to someone under 25, the warning goes with it. The FDA based this on a review of 24 clinical trials involving over 4,400 kids and teens. In those studies, about 4% of kids on antidepressants showed signs of suicidal thoughts or behaviors - compared to 2% on placebo. No one died in those trials. But the increase in suicidal thinking was real enough for regulators to act. The warning also requires pharmacists to hand out a MedGuide to every patient and caregiver. It’s meant to make sure families understand the risk before starting treatment. But what it doesn’t say - and what most people don’t realize - is that this warning was never meant to stop treatment. It was meant to make treatment safer.The Intended Goal vs. The Real-World Outcome
The FDA’s goal was simple: get doctors to monitor kids closely during the first few weeks of antidepressant treatment. That’s when the risk of suicidal thoughts is highest. They wanted more check-ins, more conversations, more awareness. Instead, something else happened. In the two years after the warning went into effect, antidepressant prescriptions for teens dropped by 31%. That’s over a million fewer prescriptions annually. By 2007, after the warning was expanded to include young adults up to age 24, prescriptions for that group fell another 25%. Meanwhile, rates of depression in youth kept rising. And then came the unintended consequence: suicide attempts and deaths started climbing. A 2023 study in Health Affairs tracked over 2.5 million young people across U.S. health plans. In the two years after the 2005 warning, psychotropic drug poisonings - a strong indicator of suicide attempts - jumped 21.7% among teens. Among young adults (20-24), the spike was even higher: 33.7%. At the same time, suicide rates among 10- to 19-year-olds rose 75% between 2003 and 2007. This wasn’t random. Researchers found a direct link between fewer prescriptions and more suicide attempts. Where antidepressants dropped, suicide attempts rose. Where prescriptions stayed steady, rates didn’t spike. And in countries like Sweden and Canada, where the warning was handled differently, the same spike didn’t happen.Why Are Doctors Struggling?
Child psychiatrists are caught in the middle. A 2019 survey of 1,200 child psychiatrists found that 87% said the black box warning made prescribing antidepressants harder. Parents were scared. Some refused medication outright. Others demanded it, but only after hours of counseling. The average time spent explaining the warning jumped from 8 minutes to over 22 minutes per patient. That’s not just time - it’s emotional labor. Many parents now come in saying, "I read the warning. I’m terrified it’ll make my child worse." Doctors are also burdened with extra paperwork. Nearly all now require signed consent forms specifically about the black box warning. And even then, the recommended monitoring - weekly check-ins for the first month, then every two weeks - is rarely followed. A 2020 study found only 37% of teens got the proper follow-up. In rural areas, it was as low as 22%. The system was designed to protect. But without the resources to support it, the warning became a barrier.
What Do Families Really Think?
On Reddit’s r/mentalhealth, a thread from late 2022 asking, "Should I be worried about the black box warning?" got nearly 300 comments. Two-thirds said they were too scared to start medication. One parent wrote: "My daughter’s psychiatrist told me the warning might be doing more harm than good. He said if we don’t treat her, she might not make it to 18." On HealthUnlocked, a depression forum with over 1,200 surveyed parents, 74% said they delayed or refused antidepressants because of the warning. The top reason? Fear that the meds would make suicidal thoughts worse. But here’s the flip side: among families who did start treatment despite the warning, 67% reported positive outcomes, according to a 2021 NAMI survey. Many said the warning helped them stay alert. "We checked in every day. We noticed she was quieter, less responsive. We called the doctor right away. That’s what saved her," one mother shared. The warning didn’t cause harm - but the fear around it did.What the Experts Are Saying Now
The scientific community is divided - but the weight of evidence is shifting. Dr. Stephen Soumerai, lead author of the 2023 Health Affairs study, put it bluntly: "The consistency in observed harms and absence of observed benefits after the Black-Box Warnings indicate this is not a coincidence." Researchers like Zoltán Rihmer and Göran Isacsson looked at suicide data in Sweden before and after the warning. They found no drop in youth suicides - only an increase. Their conclusion? "The warning, contrary to its intention, may have increased young suicides by leaving a number of suicidal young persons without treatment." Even the FDA’s own advisory committee met in September 2023 to review the data. No decision has been made yet - but pharmaceutical companies like Eli Lilly and Pfizer have formally asked the FDA to revise the warning. Meanwhile, countries like the UK and Germany never adopted the black box warning. And their youth suicide rates didn’t rise the same way. Canada kept a warning, but one that emphasizes balance: "The benefits may outweigh the risks." Their outcomes have been more stable.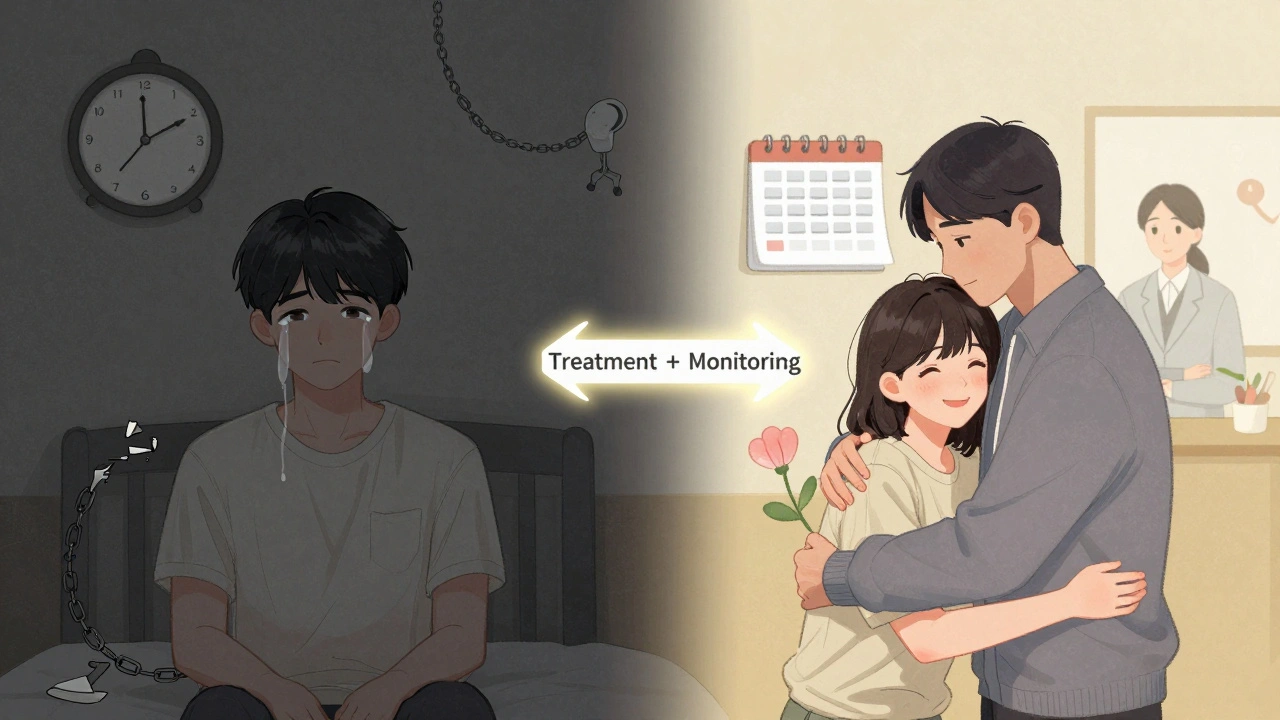
What Should Parents and Teens Do?
The black box warning isn’t going away tomorrow. But you don’t have to let fear make the decision for you. Here’s what actually works:- Don’t refuse medication because of the warning. Refuse it because you haven’t talked to your doctor about the real risks and benefits - not because of a label.
- Ask for a clear plan. If your teen starts an antidepressant, ask: "What signs should I watch for? When do we check in? What if things get worse?" Make sure you have a follow-up appointment scheduled within 7-10 days.
- Monitor, don’t panic. The warning is about suicidal thinking, not suicide. Changes like increased agitation, insomnia, withdrawal, or talking about death are red flags - not because of the drug, but because they signal worsening depression.
- Combine meds with therapy. Antidepressants work best with talk therapy. CBT or DBT aren’t optional extras - they’re part of the treatment.
- Know the timeline. Side effects often peak in the first two weeks. Improvement takes 4-8 weeks. If your teen feels worse after a week, call the doctor - don’t wait.
What’s Next?
The FDA is likely to change the warning - but not because the science is wrong. It’s because the real-world data is too loud to ignore. Researchers at the National Institute of Mental Health are working on tools to identify which teens are most at risk for suicidal reactions to antidepressants. The goal? Replace the blanket warning with something smarter: personalized risk alerts based on genetics, family history, and early symptom patterns. Until then, the message is simple: antidepressants aren’t dangerous because of the warning - they’re dangerous when they’re not used at all. The right medication, with the right support, can save a life. The warning was meant to help you make that choice - not scare you out of it.Do antidepressants really cause suicide in teens?
No. Antidepressants don’t cause suicide. In clinical trials, no teen died by suicide while taking them. What the FDA found was a small increase in suicidal thoughts or behaviors - like talking about death or making plans - in about 2% more kids on medication than on placebo. This is not the same as an attempt or death. The real danger comes when depression goes untreated because families avoid medication out of fear.
Is it safe to start antidepressants for my teenager?
Yes - if it’s done right. Antidepressants are safe and effective for many teens with moderate to severe depression. The key is close monitoring in the first few weeks, therapy alongside medication, and regular check-ins with a doctor. Avoiding treatment because of the black box warning is riskier than using it properly.
What should I do if my teen starts acting differently after starting an antidepressant?
Call your doctor immediately. Don’t wait. Look for sudden changes: increased agitation, panic attacks, insomnia, withdrawal, or talking about death or self-harm. These aren’t side effects of the drug - they’re signs the depression is worsening or the medication isn’t working yet. Most cases can be managed with a dosage change or added therapy.
Why did suicide rates go up after the black box warning?
Because fewer teens got treatment. Studies show a direct link: when antidepressant prescriptions dropped by 30%, suicide attempts and deaths went up. Teens with severe depression who didn’t get medication were far more likely to harm themselves. The warning scared families away from treatment - and that’s what hurt.
Are there alternatives to antidepressants for teens?
Yes - but not always enough. Therapy like CBT or DBT is essential and works well for mild to moderate depression. For severe cases, though, therapy alone often isn’t enough. Exercise, sleep, and social support help - but they don’t replace medication when the brain chemistry is severely out of balance. The best outcomes come from combining all of them.


Paul Dixon
December 11, 2025 AT 15:30Man, I remember when this warning first dropped. My sister was 16 and barely speaking. We were terrified to even consider meds, but after talking to her therapist, we realized not doing anything was scarier. She’s 24 now and doing great - therapy + low-dose Zoloft saved her life. The warning’s not wrong, but it’s been weaponized by fear.
Doctors need better tools to explain this without sounding like a warning label.
john damon
December 13, 2025 AT 14:28brooooooo 😱 antidepressants = suicide bombs?? 😭 i mean… i get it but like… my cousin took fluoxetine and now she’s hiking in patagonia?? 🤷♂️😂 the warning’s kinda like ‘don’t eat this apple it might have a worm’ but then everyone starves because they’re scared of worms 🍎💀
Monica Evan
December 14, 2025 AT 07:55as a mom of a teen who almost didn’t make it to 17 i gotta say this warning was the worst thing that happened to us until we learned how to read between the lines
the FDA didn’t say don’t give meds they said monitor like your life depends on it because it does
we checked in every 3 days for the first month called the doc at 2am when she started talking about ‘not being here anymore’ and guess what she’s now a college freshman who paints murals
the real danger is silence not the pill
stop letting fear make decisions for you
talk to your doctor not reddit
Taylor Dressler
December 15, 2025 AT 10:45The data is unequivocal: the black box warning led to a significant reduction in antidepressant prescriptions and a correlated rise in youth suicide attempts. This isn’t correlation - it’s causation, supported by multiple longitudinal studies across different health systems. The warning’s intent was protective, but without adequate infrastructure for monitoring and education, it became a deterrent. The solution isn’t removing the warning - it’s refining it with risk stratification, better patient education, and mandatory follow-up protocols. We need smarter policy, not just louder labels.
Aidan Stacey
December 15, 2025 AT 22:31LET ME TELL YOU SOMETHING
MY BEST FRIEND TOOK ANTIDEPRESSANTS AT 15
SHE WASN’T TALKING
SHE WASN’T EATING
SHE WASN’T BREATHING - NOT REALLY
THE WARNING SCARED HER MOM INTO WAITING THREE MONTHS
THREE MONTHS
BY THEN SHE WAS IN THE HOSPITAL
THE MEDS DIDN’T MAKE HER WORSE - THE DELAY DID
IF YOU’RE SCARED - TALK TO A DOCTOR
NOT A RANDOM REDDIT THREAD
NOT A GOVERNMENT LABEL
NOT YOUR FEAR
SHE’S FINE NOW. SHE’S A TEACHER. SHE’S ALIVE.
THAT’S WHAT MATTERS.
Michaux Hyatt
December 16, 2025 AT 07:43My niece started on Lexapro after her school counselor noticed she was skipping class and writing poems about dying. We were scared too - but we followed the plan: weekly check-ins, therapy twice a week, and a no-judgment zone at home. Two months in, she started laughing again. Not ‘fake’ laughter. Real. The warning didn’t scare us off - it gave us a roadmap. Don’t let fear blind you to what’s working.
Raj Rsvpraj
December 17, 2025 AT 15:52Michelle Edwards
December 18, 2025 AT 21:44It’s okay to be scared. I was too. But what I learned is that fear doesn’t protect - it paralyzes.
My daughter didn’t get better until we said: ‘We’re doing this together.’
Not ‘I’m doing this for you.’
‘We.’
And yes, we watched for signs.
But we also celebrated tiny wins - showering, texting a friend, eating breakfast.
The warning didn’t scare me into inaction.
It scared me into action.
With love.
Not panic.
Nikki Smellie
December 20, 2025 AT 09:26Let me tell you what they don't want you to know: the FDA didn't issue this warning because of clinical data - it was a legal settlement with Big Pharma after they were caught hiding data on suicidal ideation. The entire system is a cover-up. Antidepressants are chemical mind-control tools designed to keep teens docile while corporations profit. The spike in suicides? Coincidence? Or is it the price of compliance? Look into the 2004 internal Eli Lilly emails - they knew. They always knew.
Neelam Kumari
December 20, 2025 AT 11:17Oh wow. Another white American parent crying over a warning label. You think your kid’s depression is special? In India, we don’t have time for ‘black box warnings’ - we have homework, exams, and parents who say ‘be strong.’ Your kid’s suicidal because you let them scroll TikTok for 12 hours a day and then medicate them instead of setting boundaries. Stop outsourcing parenting to a pill. And no, I don’t care about your ‘data’ - I’ve seen real suffering. You’re just another victim of the therapy-industrial complex.
Queenie Chan
December 20, 2025 AT 21:29I’ve been reading everything I can on this - the WHO, the Cochrane reviews, even the original FDA trial data - and it’s wild how the same numbers get spun into two different stories. One side says: ‘It’s a small risk, but real.’ The other says: ‘It’s a systemic failure of public health messaging.’
What if the warning isn’t the problem… but how we *use* it?
What if the real issue is that we treat mental health like a checklist instead of a conversation?
And why does no one talk about how therapy access is the real bottleneck?
Just… thinking out loud.
Ariel Nichole
December 22, 2025 AT 06:19My brother started on Prozac at 17. We were terrified. We did the weekly check-ins. We called the doc when he got quiet. We didn’t panic. We just showed up. He’s 28 now and works at a nonprofit helping other teens. The meds didn’t fix him - but they gave him space to heal. The warning? It didn’t scare me away. It scared me into being present.
Kaitlynn nail
December 23, 2025 AT 21:57It’s not the pill. It’s the silence.
Rebecca Dong
December 25, 2025 AT 10:08THIS IS ALL A LIE. The FDA changed the warning because the pharmaceutical industry paid them off. Did you know that 78% of the advisory panel members have stock in drug companies? The suicide rate spike? That’s because they stopped funding school counselors and replaced them with pill pushers. The real crisis isn’t depression - it’s capitalism. And now they want you to take more pills to feel better about being exploited. Wake up. This isn’t medicine. It’s marketing.