Carbamazepine Medication Interaction Checker
Check for Interactions with Carbamazepine
Carbamazepine is a strong CYP3A4 inducer that can significantly reduce levels of many common medications. This tool helps identify potential interactions and their severity.
Carbamazepine isn’t just another seizure medication. It’s a silent disruptor in your body’s drug metabolism system, quietly turning up the volume on enzymes that break down dozens of other medicines you might be taking. If you’re on carbamazepine-or thinking about it-you need to understand how it changes the game for everything else in your pillbox. This isn’t theoretical. People have had unplanned pregnancies, dangerous blood clots, and sudden seizures because their other drugs stopped working. And the worst part? It doesn’t happen right away.
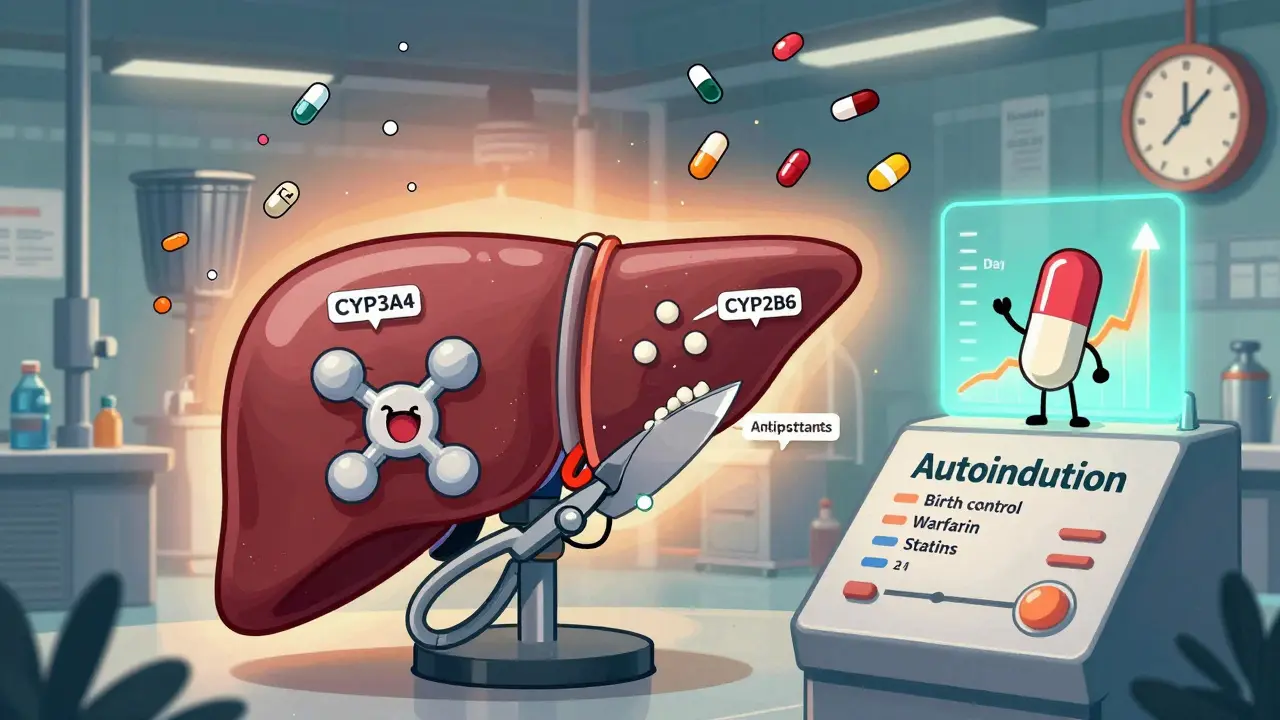
How Carbamazepine Turns Your Liver Into a Drug-Processing Factory
Carbamazepine doesn’t just sit there and work. It tells your liver to build more of a specific set of enzymes-mainly CYP3A4 and CYP2B6-that act like molecular scissors, cutting apart other drugs so your body can flush them out. This isn’t a minor effect. It’s powerful. Carbamazepine is classified by the FDA as a strong CYP3A4 inducer, meaning it can slash the levels of other drugs by 60% to 80%. That’s not a typo. A drug that used to work perfectly might become useless.
What makes carbamazepine especially tricky is that it does this to itself. This is called autoinduction. When you start taking it, your body slowly ramps up its ability to break it down. Within three to four weeks, your carbamazepine levels drop by 30% to 50%. That’s why doctors often start patients on low doses and slowly increase them. If you don’t adjust, you might think the drug isn’t working-and end up with breakthrough seizures because your blood levels fell below the therapeutic range of 4-12 µg/mL.
Doctors track this with blood tests. The American Academy of Neurology recommends checking carbamazepine levels at baseline, then again at two and four weeks after starting or changing the dose. It’s not optional. Skipping these checks is like driving without a fuel gauge.
The Medications That Stop Working-And Why
Carbamazepine doesn’t pick favorites. It hits a wide range of drugs across multiple classes. Here’s what you need to watch for:
- Birth control pills: Ethinyl estradiol levels can drop by 50% to 70%. That’s not a small risk. There are documented cases of women getting pregnant while on the pill and carbamazepine. Even if you’ve been on birth control for years, adding carbamazepine can break its effectiveness. Alternative contraception-like IUDs or implants-is strongly recommended.
- Warfarin: This blood thinner gets broken down faster. Your INR (a measure of blood clotting time) can drop dangerously low. In some cases, warfarin doses had to be increased by 50% to 100% just to stay in the safe range. Without monitoring, you could develop a clot and not know it until it’s too late.
- Antidepressants: SSRIs like sertraline and SNRIs like venlafaxine are metabolized by CYP2B6 and CYP2C19. Their levels can fall, making depression or anxiety worse. Some patients report feeling like their medication stopped working after starting carbamazepine-this is why.
- Immunosuppressants: Drugs like cyclosporine and tacrolimus are critical for transplant patients. Carbamazepine can reduce their levels by up to 60%, risking organ rejection. These patients need weekly blood tests during the first month of combination therapy.
- Statins: Simvastatin and atorvastatin are broken down by CYP3A4. Studies show simvastatin’s blood levels drop to just 26% of normal when taken with carbamazepine. That means the cholesterol-lowering effect is nearly gone. Pravastatin or rosuvastatin are safer choices.
- Benzodiazepines: Alprazolam, diazepam, and clonazepam lose potency. Patients report increased anxiety or panic attacks after starting carbamazepine-not because their condition worsened, but because the anti-anxiety drug stopped working.
Perucca et al. studied over 2,400 people on carbamazepine and found that nearly 4 out of 10 needed dose changes because of interactions. The biggest culprits? Anticoagulants, antidepressants, and immunosuppressants.
Why Carbamazepine Is Harder to Manage Than Other Inducers
There are other strong enzyme inducers, like rifampin. But carbamazepine has unique problems. Rifampin works fast-maximal induction in five days. Carbamazepine takes at least 14 days. That delay means interactions sneak up on you. You might start a new drug, feel fine for two weeks, then suddenly crash when carbamazepine finally kicks in.
Also, carbamazepine’s own metabolism changes over time. While rifampin’s effect is stable, carbamazepine’s autoinduction means the drug is constantly shifting under your feet. One study showed its clearance increased from 0.065 L/h/kg to 0.095 L/h/kg after just a few weeks. That’s a 46% jump. No other common antiseizure drug does this.
Even compared to phenytoin-another old-school enzyme inducer-carbamazepine is more aggressive against CYP3A4. It reduces midazolam (a CYP3A4 probe drug) levels by 74%, while phenytoin drops them by 64%. That difference matters in real life.

What Happens When You Stop Carbamazepine
Stopping carbamazepine doesn’t fix the problem-it flips it. Once you stop, your liver enzymes slowly return to normal. But the drugs you were taking alongside it? They’re still being cleared at the same fast rate. That means their levels can spike, leading to toxicity.
There are documented cases of alprazolam toxicity after carbamazepine was discontinued. Patients developed extreme drowsiness, confusion, and even respiratory depression because their bodies suddenly stopped breaking down the benzo as quickly. The same can happen with antidepressants, statins, or immunosuppressants.
Doctors must taper the other drugs down by 25% to 50% over two to four weeks after stopping carbamazepine. It’s not just about the seizure control-it’s about preventing overdose from drugs that are now building up in your system.
Real-World Stories Behind the Numbers
Reddit threads from r/neurology and r/pharmacy are full of stories that textbooks don’t capture. One nurse described a patient who had a seizure two weeks after starting carbamazepine. The doctor thought the dose was too low. It wasn’t. The patient’s carbamazepine level had already dropped 40% due to autoinduction. Another case involved a woman who got pregnant while on birth control and carbamazepine. She didn’t know the interaction existed. Neither did her OB-GYN.
Pharmacists report that new prescribers often miss the autoinduction timeline. They start carbamazepine at 200 mg twice daily, see no side effects, and assume it’s fine. Then, a month later, the patient comes back with worsening symptoms. By then, it’s too late to avoid a crisis.

What’s Changing? New Options and Better Tools
Carbamazepine is still widely used. In 2022, there were over 4 million prescriptions in the U.S. But its future is uncertain. Newer drugs like eslicarbazepine are being developed. Early data shows they have 80% less enzyme-inducing effect. That’s huge. If approved, they could replace carbamazepine for many patients.
There’s also a new extended-release version of carbamazepine-carbamazepine-ASP-approved by the FDA in 2023. It delivers more stable blood levels and reduces interaction potential by 30%. It’s not a cure, but it’s progress.
Researchers are also exploring genetic testing. Variations in the PXR and CAR receptors (the switches carbamazepine flips) can predict how strongly someone will induce enzymes. A clinical trial (NCT05678901) is now testing whether personalizing doses based on genetics can reduce interaction risks. It’s early, but it could change how we prescribe this drug.
What You Should Do Now
If you’re on carbamazepine:
- Make a full list of every medication you take-prescription, over-the-counter, supplements, and herbal products.
- Ask your doctor or pharmacist: "Which of these could be affected by carbamazepine?" Don’t assume they know. Many don’t.
- Get blood levels checked at baseline, two weeks, and four weeks after starting or changing dose.
- If you’re on birth control, switch to a non-hormonal method immediately.
- Never stop carbamazepine suddenly. Always work with your provider to adjust other meds first.
If you’re considering carbamazepine:
- Ask if there’s a safer alternative-especially if you’re on other medications.
- Ask about eslicarbazepine or carbamazepine-ASP. They’re newer, and interactions are less severe.
- Ask if therapeutic drug monitoring will be part of your care plan.
Carbamazepine saves lives. But it’s a double-edged sword. It controls seizures and mood swings-but it can also undo the effects of other life-saving drugs. The key isn’t avoiding it. It’s knowing how to manage it.
Can carbamazepine make birth control fail?
Yes. Carbamazepine can reduce the levels of ethinyl estradiol in birth control pills by 50% to 70%, making them ineffective. Women on carbamazepine should use non-hormonal contraception like IUDs or implants. Relying on pills, patches, or rings while taking carbamazepine carries a high risk of unintended pregnancy.
How long does it take for carbamazepine to start inducing enzymes?
Maximal enzyme induction takes at least 14 days, but the full effect builds gradually over 3 to 4 weeks. This is why autoinduction-where carbamazepine speeds up its own metabolism-isn’t noticeable right away. Blood levels drop over time, which is why dose adjustments are needed during the first month of treatment.
Do I need blood tests if I’m on carbamazepine?
Yes. Therapeutic drug monitoring is essential. Carbamazepine has a narrow therapeutic range (4-12 µg/mL), and its levels drop 30% to 50% in the first few weeks due to autoinduction. Blood tests at baseline, two weeks, and four weeks after starting or changing dose help prevent underdosing or toxicity.
Can I take warfarin with carbamazepine?
It’s possible, but risky. Carbamazepine lowers warfarin levels, reducing its anticoagulant effect. This increases the risk of blood clots. If both are needed, INR must be checked frequently-often weekly at first-and warfarin doses may need to be increased by 50% to 100%. Never adjust warfarin on your own.
What happens if I stop carbamazepine suddenly?
Stopping carbamazepine suddenly can cause seizures to return, but it can also lead to toxicity from other drugs. Once carbamazepine is gone, your liver enzymes slow down, causing other medications (like alprazolam, antidepressants, or statins) to build up to dangerous levels. Always reduce those other drugs by 25% to 50% over 2 to 4 weeks after stopping carbamazepine.
Are there safer alternatives to carbamazepine?
Yes. Eslicarbazepine is a newer drug that works similarly but causes 80% less enzyme induction. Extended-release carbamazepine-ASP also reduces interaction potential by 30%. Both are better choices for patients on multiple medications. Ask your doctor if one of these alternatives is right for you.

dana torgersen
January 22, 2026 AT 23:19So carbamazepine basically turns your liver into a drug-eating monster?? I mean… wow. I knew it was strong, but 60-80% reduction?? That’s not a side effect-that’s a full-on biochemical betrayal. I’ve seen people on this stuff and they’re like, ‘why is my antidepressant not working?’ and no one connects the dots…
Sue Stone
January 23, 2026 AT 15:10My aunt was on this for seizures and didn’t know her birth control was useless. She got pregnant. No one told her. It’s wild how many doctors still don’t bring this up.
Andrew Smirnykh
January 24, 2026 AT 03:51This is one of those posts that makes you realize how fragile our pharmacological balance is. We treat drugs like they’re static, but the body’s metabolism is a living, breathing system that adapts-and carbamazepine forces it to adapt in dangerous ways. It’s not just about dosing. It’s about systems thinking.
Stacy Thomes
January 25, 2026 AT 03:02STOP TAKING BIRTH CONTROL PILLS IF YOU’RE ON CARBAMAZEPINE. I MEAN IT. I’VE SEEN IT. WOMEN THINK THEY’RE SAFE. THEY’RE NOT. GET AN IUD. NOW. YOUR FUTURE SELF WILL THANK YOU.
Susannah Green
January 25, 2026 AT 07:52Just a heads-up: if you’re on carbamazepine and taking statins, switch to pravastatin or rosuvastatin. Simvastatin is basically useless with it. I’m a pharmacist and I see this all the time-patients come in with LDLs through the roof because they didn’t know. Also, check your levels at 2 and 4 weeks. Don’t wait for symptoms. Prevention > reaction.
Kerry Moore
January 25, 2026 AT 15:41Thank you for this comprehensive and clinically grounded summary. The emphasis on therapeutic drug monitoring is particularly critical. In my experience as a clinician, the most common failure point is not patient nonadherence, but provider ignorance regarding the time-dependent nature of enzyme induction. This deserves wider dissemination.
Oladeji Omobolaji
January 25, 2026 AT 20:14Man, I’m from Nigeria and we use this drug a lot here because it’s cheap. But no one talks about interactions. My cousin was on it for epilepsy and got a clot because his warfarin stopped working. Nobody knew why. This info needs to reach places where meds are scarce and education is too.
Janet King
January 26, 2026 AT 10:35Autoinduction is the silent killer here. Most prescribers think if the patient feels fine at week one, they’re fine. But the drop doesn’t happen until week three. That’s when the seizures return. Blood levels aren’t optional. They’re mandatory. Period.
Laura Rice
January 27, 2026 AT 00:06My therapist put me on carbamazepine for mood swings and I felt like my antidepressant just… vanished. I thought I was failing. Turns out my brain was just clearing it too fast. I cried for a week. No one warned me. Please, if you’re reading this and you’re on this med-ask your doc about your other meds. You’re not crazy. It’s the chemistry.
charley lopez
January 28, 2026 AT 12:53The CYP3A4 induction profile of carbamazepine is quantitatively distinct from phenytoin and rifampin, with a delayed time-to-maximal induction and significant autoinduction kinetics. The clinical implication is that concomitant medications metabolized via CYP3A4, CYP2B6, and CYP2C19 require proactive dose titration and serial TDM. Failure to do so constitutes a preventable iatrogenic risk.
Kerry Evans
January 29, 2026 AT 22:16People who don’t get blood tests while on carbamazepine are just asking for disaster. It’s not complicated. Check levels. Switch birth control. Don’t be lazy. This isn’t a suggestion-it’s a survival protocol. If you’re not doing this, you’re endangering yourself and others.
Vanessa Barber
January 30, 2026 AT 19:33Yeah but isn’t this just fearmongering? I mean, people have been on this for decades. Maybe the real issue is that we’re overmedicating everything else?
Dawson Taylor
February 1, 2026 AT 15:23Carbamazepine doesn’t break drugs. It reveals how fragile our assumptions are about pharmacology. The body adapts. Systems interact. Control is an illusion. The real treatment isn’t the pill-it’s awareness.
Sallie Jane Barnes
February 2, 2026 AT 08:13Thank you for writing this. I wish I’d read it before my mom’s transplant team almost lost her organ because no one told them about the carbamazepine interaction. We were lucky. Others aren’t. Please share this with anyone you know on antiseizure meds. It could save a life.