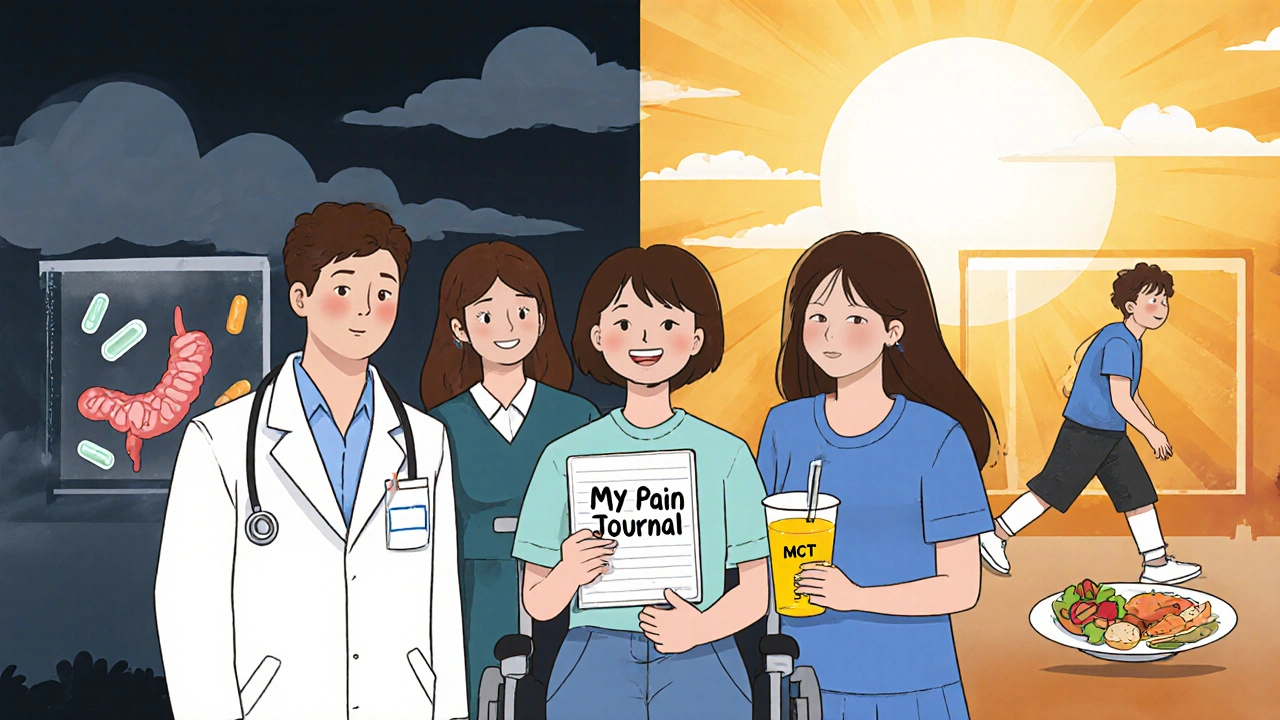
Chronic pancreatitis isn’t just a diagnosis-it’s a daily battle. For most people living with it, pain is constant, meals are risky, and even basic activities feel like a gamble. Unlike acute pancreatitis, which comes on suddenly and often resolves, chronic pancreatitis is a slow, relentless breakdown of the pancreas. The organ loses its ability to digest food and regulate blood sugar. And while there’s no cure, there are ways to take back control-if you know where to start.
Pain That Won’t Quit
Eight out of ten people with chronic pancreatitis live with persistent abdominal pain. It’s not the kind that goes away with ibuprofen. This pain is deep, burning, or stabbing, often radiating to the back. It flares after eating, especially fatty meals, and can last for hours-or days. Some describe it as a vice tightening around their midsection. Others say it feels like a knife twisting inside.
Doctors use a step-by-step approach called the WHO pain ladder. It starts simple: acetaminophen (up to 4,000 mg daily) for mild pain. If that doesn’t help, the next step is often gabapentin or pregabalin. These aren’t painkillers in the traditional sense-they calm overactive nerves. In clinical trials, they reduced pain by 40-50% in patients with nerve-related discomfort. Amitriptyline, an old-school antidepressant, works similarly for about half of users, even if they’re not depressed.
When those fail, tramadol becomes the go-to opioid. It’s weaker than morphine but less likely to cause addiction-though it still carries risk. About 30% of patients eventually need stronger opioids, but doctors hesitate. Long-term opioid use leads to dependence in 25-30% of cases, according to European guidelines. That’s why many now turn to nerve blocks. A celiac plexus block, where alcohol or steroids are injected near the nerves feeding the pancreas, gives 50-60% of patients relief for 3 to 6 months. One patient in Alberta reported nine months of near-zero pain after the procedure.
Enzyme Therapy: More Than Just Pills
When the pancreas stops making digestive enzymes, food passes through undigested. The result? Weight loss, greasy stools, bloating, and nutrient deficiencies. That’s where pancreatic enzyme replacement therapy (PERT) comes in. You don’t just take pills-you take them right with the first bite of every meal. Miss the timing, and the enzymes won’t work.
Dosing is tricky. Most people need 25,000 to 80,000 lipase units per meal. That’s often 6 to 12 capsules a day. Brands like Creon®, Zenpep®, and Pancreaze® are common, but they’re expensive-$300 to $1,200 a month without good insurance. Many patients stop taking them because of cost or pill fatigue.
Not all enzymes are the same. Some are coated to survive stomach acid. If you’re on an uncoated version, you’ll also need a proton pump inhibitor like omeprazole to protect the enzymes. Studies show high-dose PERT reduces pain in 45% of patients, likely because better digestion means less irritation in the pancreas. But effectiveness drops in advanced disease-only 30-40% of those with severe damage benefit.
There’s new hope. A 2023 enzyme called LipiGesic™ uses pH-sensitive technology to release enzymes exactly where they’re needed. In trials, it improved fat absorption by 20%. It’s not widely available yet, but it’s a sign the field is moving forward.

What to Eat-and What to Avoid
For years, low-fat diets were the gold standard for chronic pancreatitis. The idea was simple: less fat = less pain. But evidence is mixed. Some people feel better cutting fat to 40-50 grams a day. Others find it doesn’t help at all. The truth? It’s individual.
Medium-chain triglycerides (MCTs) are a game-changer. Unlike regular fats, MCTs don’t need pancreatic enzymes to be absorbed. They go straight to the liver for energy. Products like Peptamen® contain MCTs and hydrolyzed proteins. In a small 2010 study, patients drinking three cans a day saw a 30% drop in pain after 10 weeks. Many now use MCT oil-add a tablespoon to smoothies or soups.
Antioxidants might also help. A 2013 study gave patients a daily mix of selenium, vitamin C, vitamin E, beta-carotene, and methionine. After six months, 52% had less pain compared to just 23% on placebo. It’s not a magic pill, but for some, it’s a meaningful shift.
Don’t forget vitamins. About 60% of people with chronic pancreatitis are deficient in fat-soluble vitamins A, D, E, and K. Your doctor should check these every 6 to 12 months. Low vitamin D? That’s linked to worse pain. Low vitamin K? That can mess with blood clotting. Supplements are often needed.
When Medications and Diet Aren’t Enough
Some people hit a wall. Pain keeps coming back. Enzymes don’t help. Weight keeps dropping. That’s when surgery enters the picture.
Endoscopic procedures like ERCP can open blocked ducts with stents. It helps 60-70% of patients-but half of them relapse within a year. Celiac plexus blocks, mentioned earlier, are less invasive and often tried first.
Surgery is a bigger step. The Frey procedure removes part of the pancreas and connects the duct to the small intestine. It gives 70-80% of patients long-term pain relief. Total pancreatectomy with islet autotransplantation (TPIAT) removes the whole pancreas, then reimplants insulin-producing cells. It’s 85-90% effective at stopping pain. But you’ll need lifelong insulin injections.
There’s a growing push to offer surgery earlier. Dr. Melena Bellin, a leading researcher, argues that waiting too long leads to opioid dependence and depression. The goal isn’t just to stop pain-it’s to stop the spiral.
The Hidden Struggles
Behind the medical facts are real lives. On patient forums, 65% say their pain is still poorly controlled. Many spend years going from doctor to doctor before getting diagnosed. The average delay? Two to three years.
Insurance battles are brutal. High-dose enzyme therapy can cost $1,000 a month. Some insurers demand proof of malabsorption before approving coverage. Patients often skip doses or switch to cheaper, less effective brands.
Then there’s mental health. Chronic pain wears you down. Anxiety and depression are common. Yoga, as noted in a University of Pittsburgh study, improved quality of life scores by 35% in patients who practiced twice a week. Mindfulness, counseling, and support groups aren’t luxuries-they’re part of treatment.
What’s Next?
The field is changing. The NIH just launched a $15 million initiative to find better pain treatments. A new drug called cenobamate is in phase 2 trials, aiming to reduce nerve pain without opioids. Dorsal root ganglion stimulation, a type of nerve pacemaker, is showing early promise for those who’ve tried everything else.
But the biggest shift is mindset. Chronic pancreatitis isn’t just a digestive disorder. It’s a whole-body condition. Managing it means coordinating pain control, nutrition, enzyme therapy, mental health, and sometimes surgery. The best outcomes come from teams-not just one doctor.
If you or someone you know has this condition, don’t wait for pain to get worse. Ask about enzyme dosing, get your vitamins checked, explore non-opioid options, and consider a multidisciplinary pancreas clinic. You don’t have to live in constant discomfort. Better days are possible-if you know where to look.
Can chronic pancreatitis be cured?
No, chronic pancreatitis cannot be cured. The damage to the pancreas is permanent. But with proper management-enzyme therapy, pain control, diet changes, and avoiding alcohol and tobacco-many people can live well for decades. The goal isn’t to reverse the disease, but to stop it from getting worse and to manage symptoms effectively.
Do I need to take enzymes with every snack?
Yes-if the snack contains fat, protein, or carbs. Enzymes work best when taken with the first bite of food. Even a small snack like yogurt, a protein bar, or a handful of nuts can trigger digestion. Skipping enzymes leads to malabsorption, bloating, and increased pain. Most people take 2-4 capsules with snacks and 6-12 with meals, depending on fat content.
Why do I still have pain even though I’m taking enzymes?
Enzymes help with digestion and can reduce pain in about 45% of people, but they don’t fix nerve damage or inflammation. Pain in chronic pancreatitis often comes from scar tissue, duct pressure, or nerve sensitization-not just undigested food. That’s why many need additional treatments like gabapentin, nerve blocks, or even surgery. Enzymes are one tool, not a cure-all.
Is a low-fat diet always recommended?
Not always. While many people feel better on a low-fat diet (40-50g fat/day), studies show mixed results. Some patients do better with medium-chain triglycerides (MCTs), which bypass the need for pancreatic enzymes. Others find moderate fat intake works fine if they take enzymes correctly. The best approach is personalized-work with a dietitian to test what your body tolerates.
Can I drink alcohol occasionally?
No. Even small amounts of alcohol can trigger flare-ups and speed up pancreatic damage. Alcohol is the leading cause of chronic pancreatitis, responsible for 70% of cases. Stopping completely is the single most effective thing you can do to slow progression and reduce pain. Studies show 40-50% of patients experience better pain control within six months of quitting.
How do I know if my enzyme dose is right?
Look for signs: fewer greasy stools, less bloating, stable weight, and improved energy. Your doctor can order a fecal elastase test to check enzyme levels. If symptoms persist despite taking enzymes, your dose may be too low-or you may need a different formulation. Some people need up to 80,000 lipase units per meal. Don’t guess-talk to your GI specialist or dietitian about adjusting.
What vitamins should I be taking?
Most people with chronic pancreatitis need supplements for fat-soluble vitamins: A, D, E, and K. Deficiencies are common in 50-70% of patients. Your doctor should check levels every 6 to 12 months. You may also need calcium and magnesium, especially if you have diabetes. Antioxidants like selenium, vitamin C, and vitamin E may help reduce pain-ask your doctor about a specific combo based on your lab results.
Is surgery risky?
All surgery carries risks, but for severe chronic pancreatitis, the risks of not operating can be worse. Procedures like the Frey operation or TPIAT have success rates of 70-90% for pain relief. Complications include infection, bleeding, or diabetes (especially after TPIAT). But for those with uncontrolled pain and opioid dependence, surgery often restores quality of life. It’s not a last resort-it’s a valid option when other treatments fail.
If you’re struggling with chronic pancreatitis, you’re not alone. The path isn’t linear, and progress is often slow. But with the right team, the right tools, and persistence, many people find relief. Start with your enzymes, check your vitamins, stop alcohol, and ask about pain options beyond opioids. Small steps add up.


Kihya Beitz
November 15, 2025 AT 22:44Wow, another glorified drug ad disguised as medical advice. 🤡 So let me get this straight-take 12 pills with every bite, spend $1k/month on enzymes, and pray your insurance doesn’t drop you? Meanwhile, the real solution is just not drinking… but hey, let’s monetize the suffering with ‘LipiGesic™’ next quarter. I’ll stick with whiskey and duct tape, thanks.
Jennifer Walton
November 16, 2025 AT 02:44Chronic pain reshapes identity. Not just a condition-it becomes the architecture of your days. The enzymes, the blocks, the vitamins-they’re not treatments. They’re rituals. And rituals are all we have when the body betrays you silently, daily.
Ogonna Igbo
November 16, 2025 AT 09:36You Americans think you own medicine because you spend the most on it. In Nigeria we don't have Creon or PERT or nerve blocks. We use ginger, bitter leaf, and prayer. You spend $1200 a month on pills while our people die from hunger. This is not healthcare. This is capitalism with a stethoscope. Stop pretending your system is better.
BABA SABKA
November 17, 2025 AT 02:11Let’s cut through the noise. PERT isn’t a magic bullet because the pancreas isn’t a broken faucet you can just replace parts on. It’s a scarred organ drowning in fibrosis. The enzymes help digestion but don’t touch the neuroinflammation or the central sensitization-that’s why gabapentin and nerve blocks are the real MVPs. And yes, MCT oil is underrated. I’ve seen patients go from wheelchair to walking after switching to MCT-enriched shakes. The science isn’t flashy but it’s real. Stop chasing miracle drugs and start optimizing what already works.
Chris Bryan
November 17, 2025 AT 05:54Who funded this? Big Pharma? The NIH? The same people who told us opioids were safe? Now they’re pushing ‘LipiGesic™’ like it’s the next miracle. And don’t get me started on ‘mindfulness’-it’s just another way to make you accept suffering instead of fighting the system. They want you to meditate while your pancreas turns to cement. Wake up. This is all a controlled demolition of your health to sell more pills.
Jonathan Dobey
November 17, 2025 AT 13:18There’s a metaphysical layer here, you know. Chronic pancreatitis isn’t just a biological malfunction-it’s a manifestation of emotional stagnation. The pancreas? It’s the organ of digestion, yes-but also of processing what life feeds you. Unresolved grief. Suppressed rage. The refusal to let go. You take enzymes to digest food, but what are you digesting emotionally? The MCT oil? It’s not just fat-it’s a metaphor for effortless energy. The real cure isn’t in a pill bottle. It’s in surrendering to the flow. And yes, I’ve meditated through 37 flare-ups. The pain didn’t vanish. But my relationship to it? Transcended.
ASHISH TURAN
November 18, 2025 AT 08:52I have a friend with this condition. He quit alcohol, started enzymes, and now eats small meals with MCT oil. He still has pain but it’s manageable. He says the biggest help was finding a specialist who listened-not just prescribed. I think the real takeaway is: don’t give up, but don’t trust just one doctor. Keep asking. Keep pushing. And yes, check your vitamins. That one saved his life.
Ryan Airey
November 19, 2025 AT 23:04Let’s be real-this article is a PR piece for pharma. ‘LipiGesic™’? That’s not a breakthrough, that’s a patent play. The real problem? Insurance companies refuse to cover high-dose enzymes unless you prove malabsorption with a 72-hour stool test. Good luck getting that done without a $500 copay. And don’t even get me started on how they treat chronic pain patients like addicts. You’re not ‘drug-seeking’-you’re just trying to survive. The system is broken. The science? Half-baked.
Hollis Hollywood
November 21, 2025 AT 21:45I’ve been living with this for 12 years. I’ve tried everything. The nerve blocks worked for a while. The enzymes? I took them every day for five years, then stopped because I couldn’t afford them. I lost 40 pounds. My wife cried when she saw me. But here’s the thing-when I started yoga twice a week, something shifted. Not the pain, exactly. But the weight of it. It didn’t disappear, but it didn’t own me anymore. I don’t know if it’s the breathing, the movement, or just the fact that for 45 minutes, I wasn’t thinking about my pancreas. Maybe that’s enough. Maybe healing isn’t about fixing the organ. Maybe it’s about reclaiming the self.
Aidan McCord-Amasis
November 23, 2025 AT 17:20Enzymes with every snack? 😑 I just eat protein bars and hope for the best. Also, alcohol is the devil. 🍸❌
Adam Dille
November 23, 2025 AT 17:27Y’all are overthinking this. Low-fat? MCT? Enzymes? All good. But the real MVP? Stopping alcohol. Full stop. No debate. I had a cousin who quit drinking and his pain dropped by 70% in 3 months. No pills. No blocks. Just no booze. 🤷♂️✨
Katie Baker
November 24, 2025 AT 11:16This is the most helpful thing I’ve read in years. I’ve been scared to ask my doctor about enzyme dosing, but now I feel like I have a roadmap. Thank you for writing this with so much care. You’re not just sharing facts-you’re giving people hope. And that matters more than you know. 💙