When you take a pill, inject a vaccine, or use a medical device, you expect it to be safe, effective, and consistent. That’s not luck. It’s the result of Current Good Manufacturing Practice (GMP) - a strict set of rules that every pharmaceutical, medical device, and even some food manufacturer must follow. As of 2025, these standards aren’t just paperwork. They’re the backbone of global drug safety. And they’ve changed. A lot.
What Exactly Are Current GMP Standards?
GMP stands for Good Manufacturing Practice. The "Current" part is critical. It means you can’t rely on old methods, outdated equipment, or hand-written logs. You need modern systems that prevent errors before they happen. The U.S. FDA first codified these rules in 1978 under 21 C.F.R. Parts 210 and 211, but they’ve been updated continuously - especially in 2025. The core goal? Make sure every batch of medicine you buy is identical in quality. No weak pills. No contaminated syringes. No mislabeled vials. That’s not optional. It’s the law. In Europe, it’s EU GMP (EudraLex Volume 4). In many developing countries, WHO GMP is the baseline. But the FDA and EMA are the gold standard. And right now, they’re pushing manufacturers harder than ever.The Nine Core Requirements of GMP in 2025
There are nine non-negotiable pillars. Skip one, and you risk a warning letter, a product recall, or worse - a shutdown.- Quality Management: You need a full quality system. Not just a quality department. Every person, every process, every supplier must tie back to quality. The quality unit has final say on batch release - no exceptions.
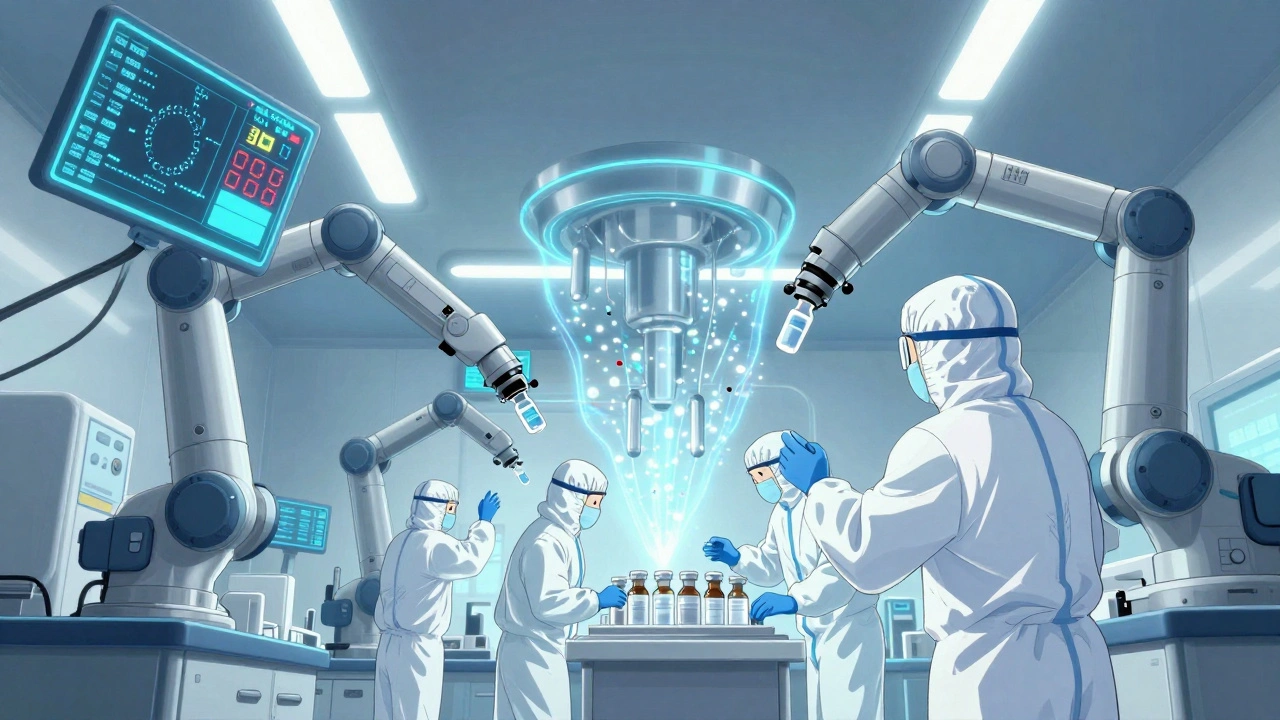
- Sanitation and Hygiene: Cleanrooms aren’t just clean. They’re monitored. Air particles? Counted. Surfaces? Swabbed. Personnel? Gowned in sterile suits. EU Annex 1 now requires full-body coverage in Grade A/B areas. No exposed skin. No exceptions.
- Building and Facilities: Layout matters. You can’t have raw materials next to finished products. Airflow must be controlled. For sterile products, you need ISO 14644-1 Class 5 cleanrooms. That’s 100 particles per cubic foot - cleaner than a hospital operating room.
- Equipment: Machines aren’t just turned on. They’re qualified. Installation Qualification (IQ), Operational Qualification (OQ), Performance Qualification (PQ) - all documented. If you replace a pump, you re-qualify it. No shortcuts.
- Raw Materials: Every ingredient is tested. Not just for identity. For potency, purity, and contamination. Temperature and humidity logs? Required. If your supplier doesn’t give you a certificate of analysis, you don’t use it.
- Personnel: Training isn’t a one-time event. It’s quarterly. Every employee must prove they know their job. And they must sign off on every step they take. If you don’t document it, it didn’t happen.
- Validation and Qualification: You can’t just say "it works." You have to prove it - repeatedly. Process validation is mandatory. If you change a mixing time, you validate it again. The FDA’s January 2025 guidance says you can’t rely on models alone. You need real-time data.
- Complaints and Recalls: If someone reports a bad batch, you have 72 hours to investigate. Root cause analysis? Required. Recalls? Must be traceable to every bottle sold. EMA says 18% of 2024 recalls were due to poor supply chain tracking.
- Documentation and Record Keeping: Everything must be written down - in real time. No backdating. No erasures. Electronic records? Must follow ALCOA+: Attributable, Legible, Contemporaneous, Original, Accurate, and + Complete, Consistent, Enduring, Available. The FDA issued 2,147 warning letters in 2024 for data integrity violations. That’s the #1 issue.
FDA vs. EU GMP: Key Differences in 2025
You can’t treat FDA and EU GMP the same. They’re not interchangeable.The FDA gives you flexibility. You decide how to meet the standard - as long as you can prove it works. That’s why U.S. companies are adopting in-line sensors, real-time monitoring, and AI-driven quality systems faster than anyone else. In 2025, 37% more U.S. plants use continuous manufacturing than in 2023.
The EU is stricter. Annex 1, which became fully effective in August 2024, demands closed isolators for sterile production. No open transfers. No manual handling. If you’re making injectables, you need robotics. And your gowning? Full-body, sterile, no gaps. The EU also requires audit trails for every change to electronic records. No one can delete or edit without a digital footprint.
Here’s the catch: companies that sell to both markets end up doing double work. One Pfizer manager told us their facility spends $75,000 a year just to meet both FDA and EU environmental monitoring requirements. It’s not efficient. But it’s necessary.
What’s New in 2025? Three Big Shifts
1. Data Integrity Is Now a Top Priority
The FDA isn’t just asking for records. They’re demanding proof they’re real. ALCOA+ isn’t a guideline - it’s an audit checklist. If your system doesn’t track who changed what, when, and why - you’re non-compliant. A PharmaTech survey found 68% of facilities struggled with this in 2024. Remediation cost an average of $185,000 per site.2. Advanced Manufacturing Is Now Expected
The FDA’s January 2025 guidance says you can replace physical sampling with in-line, at-line, or on-line measurements. That means sensors in your reactor that check pH, concentration, or particle size in real time. No more pulling vials off the line for lab tests. This reduces contamination risk and speeds up release.But there’s a catch. You can’t just install sensors. You have to validate them. And if you’re using AI to predict quality outcomes? You need to document every algorithm, every training set, every assumption. PharmUni warns that machine learning models can drift. If they’re not monitored, they become a risk - not a solution.
3. Supply Chain Oversight Is Tightening
The days of buying raw materials from unknown suppliers are over. FDA now requires risk-based supplier audits. EMA requires serialization for every prescription drug - a unique code on every package you can trace back to the batch.And it’s working. In 2024, 27% of recalls came from supplier failures. That’s up from 19% in 2022. If your supplier doesn’t have GMP certification? You can’t use their material. Period.
How Much Does It Cost to Comply?
Let’s be real. GMP isn’t cheap.For a mid-sized pharmaceutical plant, full compliance takes 18-24 months and costs about $1.2 million. That’s for upgrades, training, validation, software, and audits. Facilities with legacy equipment? Add another $250,000 per production line to retrofit sensors for in-line monitoring.
Global spending on GMP compliance hit $4.7 billion in 2024 and is growing at 8.3% a year. The pharmaceutical sector accounts for 63% of that. Medical devices are next at 22%. Food? Only 15% - but that’s growing fast.
And here’s the kicker: 92% of U.S. facilities are fully compliant with FDA standards. In the EU, it’s 78%. In emerging markets? Only 43% meet WHO GMP. That’s why drug shortages still happen - not because of lack of demand, but because of lack of compliant capacity.
What Happens If You Don’t Comply?
Warning letters. Product recalls. Import bans. Factory closures.The FDA issued 2,147 warning letters in FY2024. Most were for data integrity issues. The EMA doesn’t send as many letters, but when they do, they shut you down. One Indian API manufacturer lost its EU GMP certification in 2024 after falsifying batch records. They’re still banned.
And it’s not just regulators. Buyers - like hospitals and pharmacies - now demand proof of compliance before they’ll sign a contract. No GMP certificate? No business.
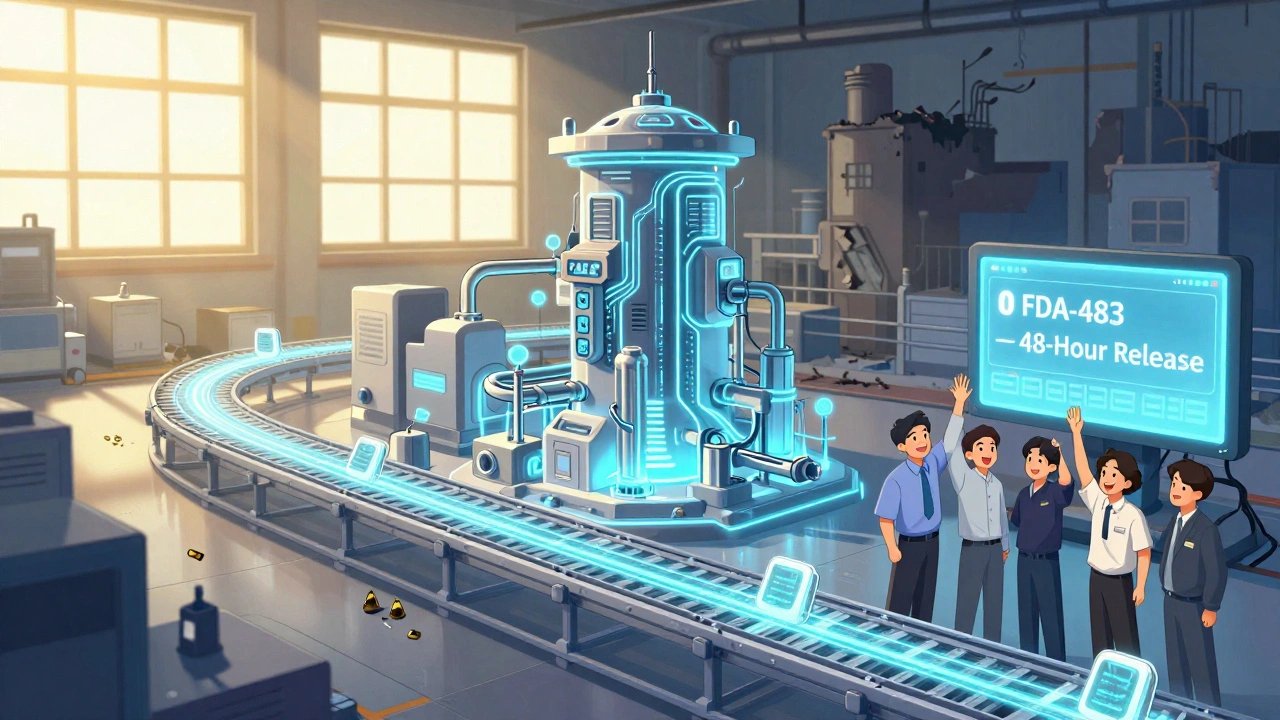
Real-World Success: Merck’s Zero-FDA-483 Facility
Merck’s Whitehouse Station plant in New Jersey is a case study in what’s possible. They moved from batch manufacturing to continuous manufacturing. They installed PAT (Process Analytical Technology) sensors throughout the line. They automated data capture. They trained everyone on ALCOA+.In 2025, they had zero FDA 483 observations - the first time in over a decade. Their batch release time dropped from 14 days to 48 hours. And their defect rate? Cut in half.
They didn’t spend more. They spent smarter.
Bottom Line: GMP Isn’t a Cost - It’s a Competitive Advantage
Yes, GMP is expensive. Yes, it’s complex. But in 2025, it’s the price of entry.Companies that treat it as a burden are falling behind. Those that treat it as a system for excellence? They’re winning. Faster approvals. Fewer recalls. Stronger trust from regulators and patients.
The future of manufacturing isn’t about cutting corners. It’s about building systems so tight, you can’t make a mistake - even if you try.
What does "Current" in CGMP actually mean?
"Current" means you must use up-to-date technology, methods, and systems. You can’t rely on 1980s equipment or handwritten logs. The FDA and EMA expect modern approaches - like real-time monitoring, automated data capture, and validated software. If your process hasn’t changed since 2010, you’re not compliant.
Can I use AI for quality control under GMP?
Yes - but only if you validate it. The FDA allows AI-driven quality prediction, but you must document every algorithm, training dataset, and decision rule. You also need ongoing monitoring to catch drift. If your AI model starts making wrong calls, you must stop using it until you fix it. PharmUni’s 2025 report warns that unvalidated AI is now one of the top risks in GMP audits.
Do I need separate GMP systems for FDA and EU markets?
Not necessarily - but you’ll likely need dual processes. The FDA allows in-line testing; the EU often requires physical sampling. The FDA accepts electronic records with ALCOA+; the EU requires full audit trails. Many companies build one system but configure it to meet both sets of rules. It’s more expensive upfront, but cheaper than running two separate facilities.
How often are GMP inspections done?
For high-risk facilities (like sterile injectables), inspections happen every 2 years. For lower-risk sites, every 3-5 years. But if you’ve had a warning letter or recall, you can be inspected again within 6 months. The FDA and EMA also do unannounced inspections more frequently now - especially since pandemic flexibilities ended in January 2025.
What’s the biggest mistake companies make with GMP?
Treating documentation as a chore instead of a control. Over 60% of FDA 483 observations in 2024 cited poor record keeping. People think, "I did it right, so why write it down?" But GMP doesn’t care what you did - it only cares what you documented. If it’s not written, it didn’t happen - and regulators will treat it like a violation.

nikki yamashita
December 12, 2025 AT 09:09Love this breakdown! Seriously, GMP isn’t just paperwork-it’s what keeps us from getting sick from a bad pill. 🙌
wendy b
December 12, 2025 AT 23:29Ok but let’s be real-most of these ‘standards’ are just corporate theater. I’ve seen labs where they print out the ALCOA+ checklist and tape it to the wall while the techs scribble notes on napkins. 😒
Adam Everitt
December 14, 2025 AT 00:29There’s a metaphysical tension here, isn’t there? We demand perfection in medicine-yet the systems meant to ensure it are built by fallible humans using flawed tools. The irony is poetic. Or tragic. Depends on your coffee intake.
Audrey Crothers
December 14, 2025 AT 20:10YES!! I work in pharma QA and this is spot on. Real-time monitoring? Game changer. My team just cut release time from 2 weeks to 48 hrs. No more all-nighters! 🎉
Stacy Foster
December 16, 2025 AT 10:31They’re lying. GMP is just a scam to make big pharma richer. The FDA takes bribes. You think they care about safety? They care about stock prices. That Merck ‘zero 483’? Probably cooked the data. I know how it works.
Reshma Sinha
December 16, 2025 AT 12:07From India-this is gold. We’re scaling up here, but supplier audits? Nightmare. One vendor sent us lactose with 3% moisture. No CoA. We rejected it. Now they’re mad. But safety first.
Lawrence Armstrong
December 17, 2025 AT 02:56AI for quality control? Totally valid-if you validate it properly. I’ve seen models drift so bad they flagged good batches as bad. GMP 2025 is about smart tech, not magic. 🤖✅
Donna Anderson
December 17, 2025 AT 09:42My boss still prints batch records. On paper. In triplicate. I swear he thinks the FDA prefers ink over electrons. 😅
sandeep sanigarapu
December 19, 2025 AT 05:35Compliance is not optional. It is the foundation. In India, we are catching up. Training, documentation, and culture matter more than tools. The tools follow the mindset.
Ashley Skipp
December 19, 2025 AT 07:09Why do we even need all this paperwork? If the medicine works who cares if someone forgot to sign a log
Nathan Fatal
December 19, 2025 AT 07:12The real question isn’t whether GMP is expensive-it’s whether we’re willing to pay the price of non-compliance. Lives. Trust. Reputation. The cost of cutting corners isn’t measured in dollars-it’s measured in deaths. And we’ve seen that number rise.
Robert Webb
December 21, 2025 AT 02:40I’ve been in this industry for 22 years, and I’ve watched GMP evolve from binders full of handwritten logs to fully integrated LIMS with blockchain-backed audit trails. The shift isn’t just technological-it’s cultural. The best facilities don’t just comply-they internalize quality. Every technician knows their role in the chain. That’s the real win.
Laura Weemering
December 21, 2025 AT 15:55ALCOA+? More like ALCOA-PLUS-OF-DOOM. I’ve spent 300 hours this year just documenting why I didn’t delete a file that didn’t exist. And the audit trail? It’s a labyrinth. I’m not a data scientist-I’m a technician. Why do I need to log my coffee break? It’s not like the pill cares if I took a sip at 10:17 a.m.
Rob Purvis
December 22, 2025 AT 01:52For anyone thinking AI is a shortcut-think again. I trained a model to predict contamination based on vibration patterns in a mixer. Worked great for 6 months. Then it started flagging normal batches as contaminated. Turned out the vendor changed the motor’s bearing type. We didn’t retrain. Big mistake. GMP doesn’t forgive lazy AI.
Levi Cooper
December 22, 2025 AT 11:43Europe’s rules are ridiculous. Why should an American company spend $75k/year just to satisfy some EU bureaucrat who thinks gloves should cover their eyebrows? We’re the ones making the medicine. Let us do it our way.