Medication Adherence Impact Calculator
Medication adherence is crucial for treatment success. This calculator shows how improving adherence can reduce hospitalizations using real-world clinical data. Based on studies showing 62% to 84% adherence improvement with digital pill systems.
Key Insight: A 22% increase in adherence (from 62% to 84%) reduced hospitalizations by 37% in a 12-week study with antipsychotic users.
For decades, doctors have known that patients often skip doses, forget to refill prescriptions, or stop taking meds altogether - especially for chronic conditions. The World Health Organization says only about half of people stick to their medication plans. That’s not laziness. It’s forgetfulness, fear, cost, or just life getting in the way. But what if your pill could tell you - and your doctor - when you actually swallowed it?
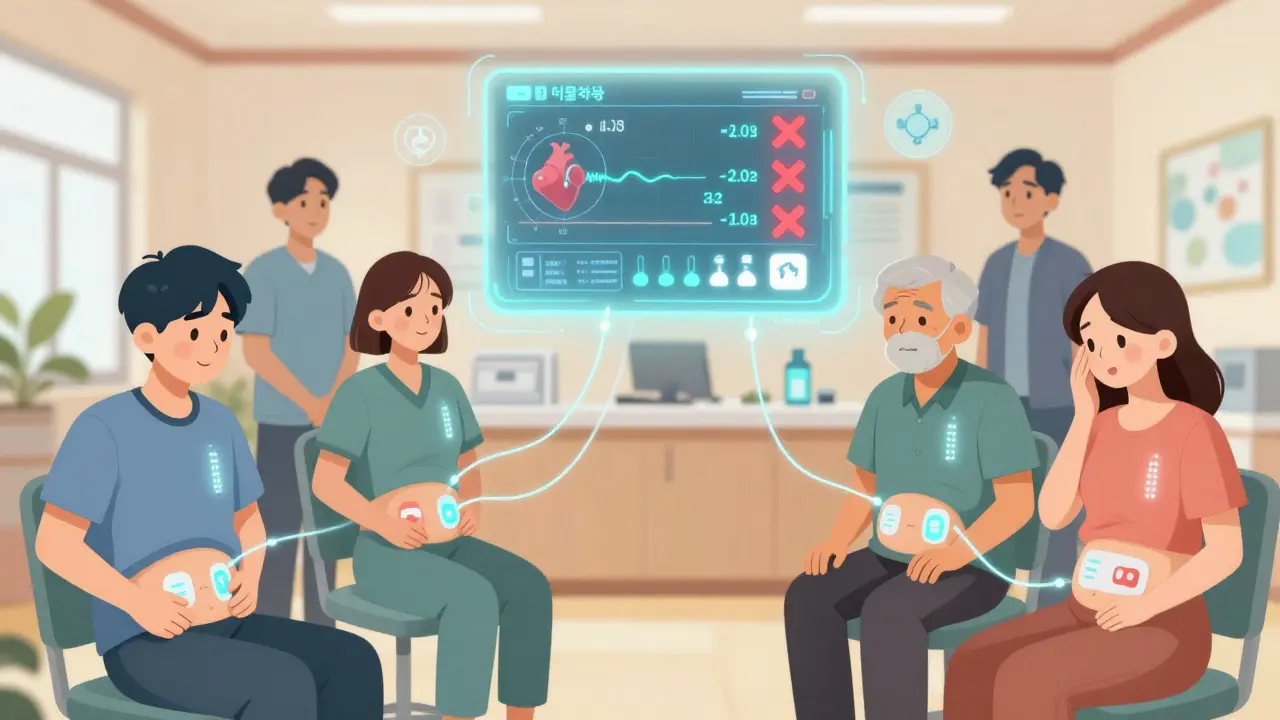
How Digital Pill Sensors Work
Digital pill sensors are tiny electronic chips embedded inside medication tablets. They’re not magic. They’re small silicon disks, about the size of a sesame seed, with copper and magnesium electrodes. When you swallow the pill, stomach acid activates the sensor. The magnesium reacts with the copper, creating a tiny electric current - just enough to send a signal. That signal gets picked up by a patch you wear on your skin, usually on your abdomen. The patch then sends the data to your phone via Bluetooth, and from there, it goes to a secure server.The system doesn’t just say, “You took the pill.” It says, “You took it at 8:14 a.m. on Tuesday.” That’s the core innovation. The first FDA-approved digital pill, Abilify MyCite, came out in 2017 for schizophrenia and bipolar disorder. Since then, systems from etectRx, Philips, and Proteus have expanded into HIV treatment, heart disease, diabetes, and even tuberculosis.
What’s surprising is how simple the tech is. No batteries inside the pill. No wires. Just chemistry and radio waves. The patch, however, needs charging. Most last about 72 hours before needing a recharge. And the app? It’s not fancy. But it shows a clean timeline: green checkmarks for taken doses, red X’s for missed ones. No fluff. Just facts.
Real-World Impact on Adherence
In clinical trials, digital pills have moved the needle. One 12-week study with 157 people on antipsychotic meds saw adherence jump from 62% to 84%. That’s not a small win. It means fewer hospital visits, less relapse, and better outcomes. One Reddit user with schizophrenia said, “Seeing my ingestion records made me realize I was skipping doses on weekends.” That’s the power of feedback. When you can see your own behavior, you change it.But it’s not universal. People with hypertension or high cholesterol - conditions that don’t feel urgent - were far less likely to use the tech. In one survey, only 42% said they’d want it for blood pressure meds. Meanwhile, 68% were open to it for serious mental illness. Why? Because the stakes feel higher. Missing a dose of Abilify can mean a psychotic episode. Missing a statin? Maybe not.
Still, 22% of users quit because the patch irritated their skin. Another 38% of older adults needed help just connecting the patch to their phone. The tech works - but only if it’s easy enough to use.
Side Effect Detection: Beyond Just Taking the Pill
The next wave of digital pills isn’t just about tracking ingestion. It’s about detecting what happens after you swallow it.Some systems, like Philips’ IntelliCap, now monitor stomach temperature and pH levels in real time. Others are testing sensors that detect specific biomarkers - chemicals your body releases when it’s reacting to a drug. Imagine this: you take your blood thinner, and within minutes, the system notices your heart rate spiked and your body temperature dropped slightly. That could signal an early sign of internal bleeding - before you even feel dizzy.
In March 2023, the FDA approved the first digital pill for tuberculosis treatment. That’s huge. TB meds require 6-9 months of daily doses. Missing even one can breed drug-resistant strains. Now, clinics can see not just if the pill was taken, but if the patient is showing signs of liver stress or nausea - common side effects of TB drugs - through physiological changes tracked by the patch.
By 2026, 60% of digital pill systems are expected to include side effect detection. That’s not sci-fi. It’s happening. Companies like etectRx are teaming up with IBM Watson Health to build AI models that predict adverse reactions based on patterns. If your pulse drops every time you take your painkiller, the system might warn your doctor before you land in the ER.
Privacy and the Cost of Being Watched
This is where things get messy.Patients love the data - until they realize someone else is seeing it. In surveys, 73% of hesitant users cited privacy as their top concern. “It feels like my psychiatrist is watching me swallow pills,” one user said. That’s not paranoia. It’s real.
Health data from these pills is protected under HIPAA - but only if it’s handled by a healthcare provider. If an insurer or employer somehow gets access, there’s little legal barrier. The Electronic Frontier Foundation warned in 2020 that this data could be used to deny coverage or raise premiums. And while most systems require patient consent to share data, the fine print often lets providers view real-time logs. That creates tension. Is this helping you - or controlling you?
Even doctors are divided. Some say it’s a lifeline for patients who’ve fallen through the cracks. Others worry about “therapeutic misconception” - patients thinking the sensor itself is curing them, not the medicine. One Stanford researcher called it a “false sense of security.”
Who’s Using This - and Who Can’t
Right now, the biggest users are pharmaceutical companies running clinical trials. About 78% of digital pill deployments are in research settings. Why? Because they need perfect data. If a new drug fails in a trial, was it because the drug didn’t work - or because patients didn’t take it? Digital pills answer that.But in clinics? Adoption is slow. Only 12% of uses are direct-to-consumer. Why? Cost and reimbursement. The pills themselves aren’t expensive - maybe $1-$2 extra per dose. But the patch, app, and data platform? That adds up. Medicare and most insurers don’t cover it yet. And without payment, doctors won’t prescribe it.
Market data shows the global digital pill industry was worth $627 million in 2022. By 2029, it’s expected to hit $2.4 billion. That growth is real - but it’s not evenly spread. Mental health leads the way (47% of uses), followed by HIV care (18%) and heart disease (15%). Diabetes and cancer trail behind. The tech works best where adherence is life-or-death - and where patients are already in regular contact with providers.

What’s Holding It Back
The tech isn’t perfect. Signal interference happens in 12-15% of cases. If you’re overweight, the signal drops even more - up to 18% failure rate for people with a BMI over 35. Sensor orientation in the stomach matters. A pill that lands sideways might not trigger the sensor properly. And even if the pill is ingested, the system can’t tell if the drug was absorbed. That’s a big blind spot.Training doctors to use the data is another hurdle. One survey found clinicians need 3-5 hours of training just to interpret the dashboards. Many don’t know what to do with the alerts. “We get a notification that a patient missed a dose,” said a nurse in Ohio. “But we don’t have time to call them. We’re already overloaded.”
And then there’s the patch. Some users get rashes. Others find it uncomfortable during workouts or showers. The 72-hour battery life means frequent recharging - and if you forget, you lose data.
The Future: Smarter, Not Just More Connected
The next step isn’t just more sensors. It’s smarter interpretation.AI is coming. etectRx’s partnership with IBM Watson Health aims to predict missed doses before they happen - using your sleep patterns, weather, activity levels, and past behavior. If you usually skip meds after a long shift, the system might send a gentle nudge the night before.
By 2026, digital pills could auto-adjust dosing. Imagine a pill that releases its contents only when your body is ready - triggered by pH levels or temperature changes. That’s already being tested in labs.
But the real question isn’t whether the tech works. It’s whether we’re ready for it. Will patients trust it? Will insurers pay for it? Will doctors know how to use it without adding more stress?
One thing’s clear: the days of guessing whether someone took their medicine are ending. The data is here. The question now is: what do we do with it?


Jason Yan
January 14, 2026 AT 19:08It’s wild to think that the same tech that tracks your steps now tracks whether you swallowed your pills. I’ve watched my uncle struggle with his antipsychotics for years - silent, ashamed, lost in the noise of his own mind. This isn’t surveillance, it’s scaffolding. For people who feel like they’re failing just by existing, seeing that green checkmark might be the only thing that says, ‘You’re still here, and that matters.’ The patch irritates? Fine. The app is clunky? Okay. But the data? That’s the quiet lifeline no one talks about. We don’t need perfect adherence. We need consistent presence. And this? This gives us a way to measure that without shame.
shiv singh
January 16, 2026 AT 14:31So now we’re gonna turn patients into data points so Big Pharma can sell more pills? Classic. You think this is helping? Nah. It’s just another way to make people feel guilty for being human. You miss a dose because you’re broke, tired, or just don’t feel like it today? Now you get a red X on your phone like you’re a bad student. Meanwhile, the drug costs $800 a month and your insurance won’t cover it. Who’s really being watched here? Not the CEOs. You.
Sarah Triphahn
January 17, 2026 AT 15:11Let’s be real - this tech is only useful for people who already care. The people who need it most? The ones who don’t show up for appointments, who can’t afford the patch, who don’t own a smartphone - they’re not even in the equation. This isn’t innovation. It’s exclusion dressed up as progress. And the side effect detection? Please. If your body’s reacting badly, you’ll know before the app does. You’ll be in the ER. Not because the sensor failed - because the system failed you first.
Vicky Zhang
January 17, 2026 AT 18:44I have a cousin with bipolar disorder and she’s been on this system for a year. I used to panic every time she didn’t answer her phone for two days. Now? I get a notification if she skips a dose. Not because I’m controlling - because I love her. And honestly? Seeing that she took her pill on her birthday last year - that tiny green dot - made me cry. It’s not about being watched. It’s about being seen. Even when you can’t say it out loud. This isn’t magic. But it’s the closest thing to a hug from a machine I’ve ever seen.
says haze
January 18, 2026 AT 17:50The fundamental flaw here is the conflation of compliance with care. Digital pills don’t improve health outcomes - they improve data fidelity. That’s not the same thing. You can have perfect adherence and still die from a drug interaction. You can have perfect data and still have a doctor who doesn’t know how to interpret it. And let’s not forget: the system can’t tell if the pill was vomited up, crushed, or dissolved in a drink. It only confirms ingestion. That’s not medical insight - it’s a digital placebo. We’re building a surveillance infrastructure on top of a broken healthcare system and calling it a solution.
Alvin Bregman
January 20, 2026 AT 02:52so like... the pill just sends a signal when its in your stomach right? so what if you swallow it but dont actually absorb it? like if you got drunk or your gut is messed up? the system thinks you took it but your body didnt get the medicine? thats kinda wild. also the patch? i sweat like a pig during workouts. imagine wearing that thing for 3 days straight. yikes. also why is this even a thing? cant we just text reminders? or put meds in pill boxes? this feels like overkill
Sarah -Jane Vincent
January 21, 2026 AT 21:01Oh please. This is just the beginning. Next they’ll put microchips in your water bottle to track hydration. Then your toothbrush to monitor brushing compliance. Then your underwear to track sleep cycles. This isn’t medicine. It’s corporate control. And guess who owns the data? Not you. Not your doctor. Some tech startup in Silicon Valley with a privacy policy written in 8-point font. They’ll sell your ingestion logs to insurers. You’ll get denied coverage because you ‘missed three doses in Q2.’ Wake up. This is the dystopia they sold us as convenience.
Henry Sy
January 22, 2026 AT 14:34Man i used to take my meds like a robot until i got the patch and it made me feel like a lab rat. i started skipping on purpose just to prove i could. like yeah i took it last week but today? nah. i’m not your data point. and the app? it’s so ugly i delete it every time. but then i forget and miss a dose and feel like crap. so i reinstall it. it’s a loop. and now i’m addicted to the red x’s like they’re some kind of punishment i deserve. this tech isn’t helping me. it’s just giving me a new way to hate myself.
Anna Hunger
January 22, 2026 AT 16:10While the technological innovation is undeniably impressive, the ethical and logistical implications remain profoundly underexamined. The assumption that behavioral data equates to therapeutic efficacy is both reductionist and dangerous. Moreover, the burden of technological literacy is disproportionately placed on vulnerable populations - elderly, low-income, neurodivergent - who are precisely the demographic most in need of support. Until reimbursement models, user-centered design, and clinician training are prioritized over data collection metrics, this innovation risks exacerbating health disparities rather than alleviating them.
Robert Way
January 23, 2026 AT 15:38wait so if the pill lands sideways it doesnt trigger? so like if i take it and it gets stuck or i swallow it wrong and the sensor dont work... then it shows i missed it? but i did take it? that seems like a huge flaw. also what if i swallow 2 by accident? does it count as one? or two? this feels like a glitchy fitness tracker but for my stomach. why is this even approved? someone needs to fix this before it hurts someone