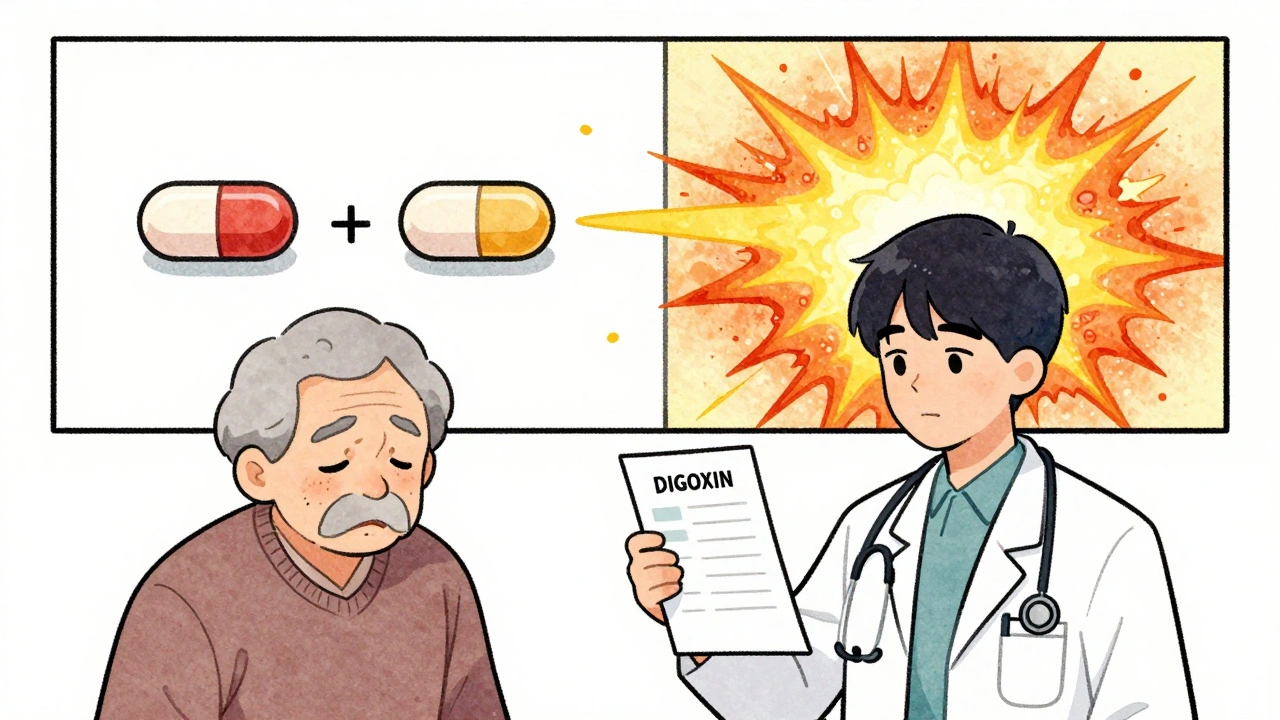
Switching from one brand of digoxin to another might seem like a simple cost-saving move - but for patients taking this medication, it can be dangerous. Digoxin is not like most pills. Even tiny changes in how much of the drug enters your bloodstream can lead to serious harm: heart rhythm problems, nausea, vision changes, or worse. This isn’t speculation. It’s why doctors and pharmacists treat digoxin differently than other generics.
Why Digoxin Is Different
Digoxin is used to treat heart failure and atrial fibrillation. It helps the heart pump more efficiently and slows down a racing heartbeat. But here’s the catch: the difference between a safe, effective dose and a toxic one is razor-thin. The therapeutic range? Just 0.5 to 2.0 nanograms per milliliter of blood. That’s less than a grain of salt in a swimming pool. Go just a little over, and you risk life-threatening arrhythmias. Go a little under, and the heart failure symptoms come back.
Because of this, digoxin is classified as a narrow therapeutic index (NTI) drug. That means even small changes in how your body absorbs the drug can have big consequences. And that’s where generic versions become tricky.
The Bioavailability Problem
Bioavailability refers to how much of the drug actually gets into your bloodstream after you swallow it. For most medications, a 20% variation between brand and generic is considered acceptable. But for digoxin? The FDA says no. To be approved, a generic digoxin tablet must match the brand-name Lanoxin within 80% to 125% for two key measurements: total exposure (AUC) and peak concentration (Cmax). That’s stricter than for most drugs.
Studies have shown that many generic digoxin products meet this standard. One 2004 study in Saudi Arabia tested a generic called Cardixin against Lanoxin in 12 healthy men. The results? The bioavailability was well within the acceptable range. Another study in Estonia found similar results. So why the concern?
Because these studies look at averages - not individuals. Let’s say 10 people take a generic digoxin. Nine of them absorb 90% of the drug. That’s fine. But the tenth person? They only absorb 45%. On paper, the average is still 84%, so the FDA says it’s bioequivalent. But for that one person, the dose is nearly half. They could go from being stable to having dangerous symptoms - all because of a switch they didn’t even know about.
Switching Between Generics Is the Real Risk
The biggest danger isn’t switching from Lanoxin to a generic. It’s switching from one generic to another. There are no studies comparing different generic brands of digoxin to each other. The FDA only requires each generic to match Lanoxin. They don’t test if Generic A is the same as Generic B.
Imagine you’ve been taking Generic A for six months. Your heart feels better. Your blood levels are steady. Then your pharmacy runs out. They give you Generic B instead. No warning. No doctor’s note. Just a different pill in the bottle.
That’s not rare. It happens all the time. One patient in a case report went from a stable digoxin level of 1.1 ng/mL to 1.8 ng/mL after switching generics - a 64% increase. They developed nausea, dizziness, and an irregular heartbeat. Dose had to be cut in half. Another patient dropped from 1.4 to 0.7 ng/mL - a 50% drop. Their heart rate spiked. They ended up in the ER.
These aren’t outliers. They’re predictable outcomes when you treat a narrow therapeutic index drug like it’s just another generic.

Why Formulation Matters Too
It’s not just about the manufacturer. The form of the drug matters too. Digoxin tablets are absorbed at about 60-80% efficiency. But the liquid form - the elixir - is absorbed at 70-85%. That means if you switch from tablet to liquid, even if it’s the same brand, your blood level can jump. The same applies if you switch from a brand-name tablet to a generic liquid. The math changes. The risk changes.
And it’s not just absorption. Some generics may dissolve differently in the stomach. A tablet that breaks down too slowly might not release enough drug. One that dissolves too fast could spike levels dangerously. These differences are invisible to the patient - but deadly in practice.
Who’s Most at Risk?
Most digoxin users are older adults. Many have kidney problems. Digoxin is cleared by the kidneys. If your kidneys slow down - which happens with age or dehydration - the drug builds up. That’s why doctors check kidney function regularly. But if you’re also switching between generics? The risk multiplies.
Patients on multiple medications are also vulnerable. Drugs like amiodarone, verapamil, or even some antibiotics can interfere with how digoxin is processed. Add a new generic on top of that? You’re stacking risk on top of risk.
What Should You Do?
If you take digoxin, here’s what matters:
- Stay on the same product. Whether it’s Lanoxin or a specific generic, try to stick with it. Don’t let the pharmacy switch you without telling you.
- Ask for the brand name. If cost is an issue, talk to your doctor. Some insurance plans cover Lanoxin for NTI drugs. Others offer patient assistance programs.
- Know your blood levels. Your doctor should check your serum digoxin level 4-7 days after starting or changing the dose. Do it again if your kidney function changes, you start a new medication, or you feel off.
- Watch for warning signs. Nausea, vomiting, loss of appetite, blurred vision (yellow or green halos), confusion, or a slow or irregular heartbeat? Call your doctor immediately. Don’t wait.
- Don’t assume generics are interchangeable. Just because two pills look the same doesn’t mean they act the same.
The Bottom Line
Digoxin generics aren’t unsafe. Many are bioequivalent to the brand. But bioequivalence doesn’t mean safety for every individual. The system was built for population averages. Digoxin needs individual precision.
That’s why the American College of Cardiology and the American Heart Association both say: use the same manufacturer’s product whenever possible. That’s not just a suggestion. It’s a safety rule.
If you’re on digoxin, your medication isn’t just about the dose. It’s about consistency. The same pill. The same manufacturer. The same routine. Because when your therapeutic window is this narrow, the smallest change can be the most dangerous one.
Monitoring Isn’t Optional - It’s Essential
Therapeutic drug monitoring isn’t a luxury for digoxin. It’s the only way to know if the pill you took actually worked. Blood levels should be checked:
- 4-7 days after starting therapy or changing dose
- After any change in kidney function
- When adding or stopping other medications
- After switching manufacturers - even if both are generics
- If you develop symptoms of toxicity or worsening heart failure
Measurements should be taken just before your next dose - the trough level. That’s when the drug is at its lowest, and it tells you if you’re building up too much.
Recent studies suggest that for heart failure patients, levels between 0.5 and 0.9 ng/mL may be safer than the old 0.5-2.0 range. Higher levels don’t mean better results - they just mean more risk.
What If You’re Already Switched?
If you’ve recently switched from one digoxin product to another - even if your doctor didn’t tell you - don’t wait. Schedule a blood test within 3-5 days. Tell your pharmacist and doctor exactly what you took before and what you’re taking now. Write it down: brand name, generic name, manufacturer, dose.
If you feel different - even slightly - get checked. Don’t assume it’s just stress or aging. It could be digoxin.
The system expects you to be passive. But with digoxin, you have to be active. Your life depends on it.
Are all digoxin generics the same?
No. While each generic must meet FDA bioequivalence standards compared to the brand-name Lanoxin, there are no studies comparing one generic to another. Two different generic brands may have different absorption rates, dissolution profiles, or inactive ingredients. Switching between them can cause dangerous shifts in blood levels.
Can I switch from brand-name digoxin to a generic safely?
It’s possible, but only if your doctor monitors your blood levels closely. Even if the generic is approved as bioequivalent, individual responses vary. Your doctor should check your serum digoxin level 4-7 days after the switch and watch for symptoms of toxicity or underdosing.
Why is digoxin more risky than other generics?
Digoxin has a narrow therapeutic index - the difference between a helpful dose and a toxic one is very small. Small changes in absorption can push levels out of the safe range. Most other drugs have wider safety margins, so minor bioavailability differences don’t cause harm. With digoxin, they do.
Should I avoid generics altogether?
Not necessarily. Many generic digoxin products are safe and effective. But you should stick with the same one. Avoid switching between manufacturers. If cost is a concern, ask your doctor about patient assistance programs or insurance coverage for the brand-name version.
How often should digoxin blood levels be checked?
Check levels 4-7 days after starting or changing the dose. Also check after any change in kidney function, new medications, or if you switch manufacturers. If you’re stable, annual checks may be enough - but only if nothing else changes. Any new symptom or change in health warrants a test.
What are the signs of digoxin toxicity?
Common signs include nausea, vomiting, loss of appetite, fatigue, confusion, blurred vision (especially seeing yellow or green halos), and irregular heartbeat. Slow heart rate (bradycardia) or new heart rhythm problems like ventricular tachycardia are serious red flags. Call your doctor or go to the ER if you notice any of these.
Is digoxin elixir more likely to cause problems than tablets?
It’s not more likely to cause problems - but it’s more predictable in absorption. The liquid form is absorbed at 70-85% efficiency, compared to 60-80% for tablets. Switching from tablet to liquid - even within the same brand - can raise your blood level. Always check levels after changing the formulation.
Can I trust my pharmacy’s generic substitution?
Not without your knowledge. In many places, pharmacists can substitute generics without telling you. Ask your pharmacist: "Is this the same manufacturer as before?" If not, contact your doctor. You have the right to request the brand or a specific generic. Don’t let cost savings override safety.


Ernie Blevins
December 7, 2025 AT 03:33This stuff scares me. My grandma switched generics and ended up in the ER with her heart going nuts. No one told her it was a risk. Just a different pill. Now she’s on Lanoxin and they won’t touch her with a ten-foot pole. Why is this even allowed?
Nicholas Heer
December 7, 2025 AT 14:24Big Pharma and the FDA are in bed together. They don’t care if you die as long as the generics cost 30% less. They test against Lanoxin but never compare generic to generic. That’s not science, that’s corporate fraud. They’re playing Russian roulette with old people’s hearts and calling it ‘cost-efficiency.’ Wake up people.
Sangram Lavte
December 8, 2025 AT 05:57As someone who works in a clinic in India, we see this often. Patients switch generics because of cost, then come back with nausea and dizziness. We now document the manufacturer name on prescriptions. Simple step. Huge difference. It’s not about being anti-generic. It’s about being smart.
Oliver Damon
December 8, 2025 AT 17:45There’s a deeper philosophical issue here. Medicine treats patients as statistical units. But biology isn’t a spreadsheet. Two people can have identical lab values and completely different experiences with the same drug. Digoxin exposes the flaw in our system: we optimize for averages, not individuals. The real tragedy isn’t the bioavailability gap - it’s that we still haven’t learned to treat people, not data points.
Stacy here
December 10, 2025 AT 08:54They’re literally gambling with people’s lives. I’ve seen patients go from stable to near-death because a pharmacist swapped generics without telling them. And the worst part? No one gets held accountable. The system is designed to let this happen. It’s not negligence - it’s policy. We need mandatory manufacturer labeling on every prescription. No more silent switches. This isn’t just medical advice - it’s civil rights.
Helen Maples
December 11, 2025 AT 02:18My mom’s on digoxin. We now call the pharmacy before every refill and ask: ‘Same manufacturer?’ If not, we call the doctor. It’s a pain, but it’s saved her from two ER trips. If you’re on this med, don’t wait for a crisis. Be the person who asks the question. You’re not being difficult - you’re being alive.
Jennifer Anderson
December 12, 2025 AT 23:14My aunt had a heart attack after switching generics. They said it was ‘just a coincidence.’ But she never had symptoms before. Now she’s on brand-name and her numbers are perfect. I’m telling everyone I know: if you’re on digoxin, write the manufacturer on your hand. Seriously. It’s that important.
Sadie Nastor
December 13, 2025 AT 13:50Thank you for writing this. I’ve been so scared to speak up because everyone says ‘generics are the same.’ But my uncle almost died from a switch. Now I carry a card in my wallet that says ‘I take digoxin - do not substitute without doctor approval.’ 😊 I wish more people knew this.
Wesley Phillips
December 13, 2025 AT 23:33