More than 1 in 10 people say they have a drug allergy. But here’s the truth: most of them don’t. If you’ve ever stopped taking a medicine because you got a rash, felt sick, or had a headache after taking it, you might think you’re allergic. You’re not alone. But confusing a side effect with a true allergy can cost you - in money, in treatment options, and even in your health.
What’s Really Happening When You React to a Drug?
Not all bad reactions to medicine are the same. There’s a big difference between a drug allergy and a side effect. One is your immune system going into overdrive. The other is just how the drug works - sometimes in ways you don’t like.
A drug allergy means your body thinks the medication is an invader - like a virus or pollen. Your immune system reacts by making antibodies, releasing histamine, and triggering inflammation. That’s what causes symptoms like hives, swelling, trouble breathing, or even anaphylaxis - a life-threatening reaction.
A side effect? That’s not your immune system. It’s the drug doing exactly what it’s supposed to do… just in a way that bothers you. For example, statins can cause muscle aches because they affect muscle cells. Antibiotics like amoxicillin can cause diarrhea because they disrupt gut bacteria. These aren’t allergies. They’re predictable, common, and often manageable.
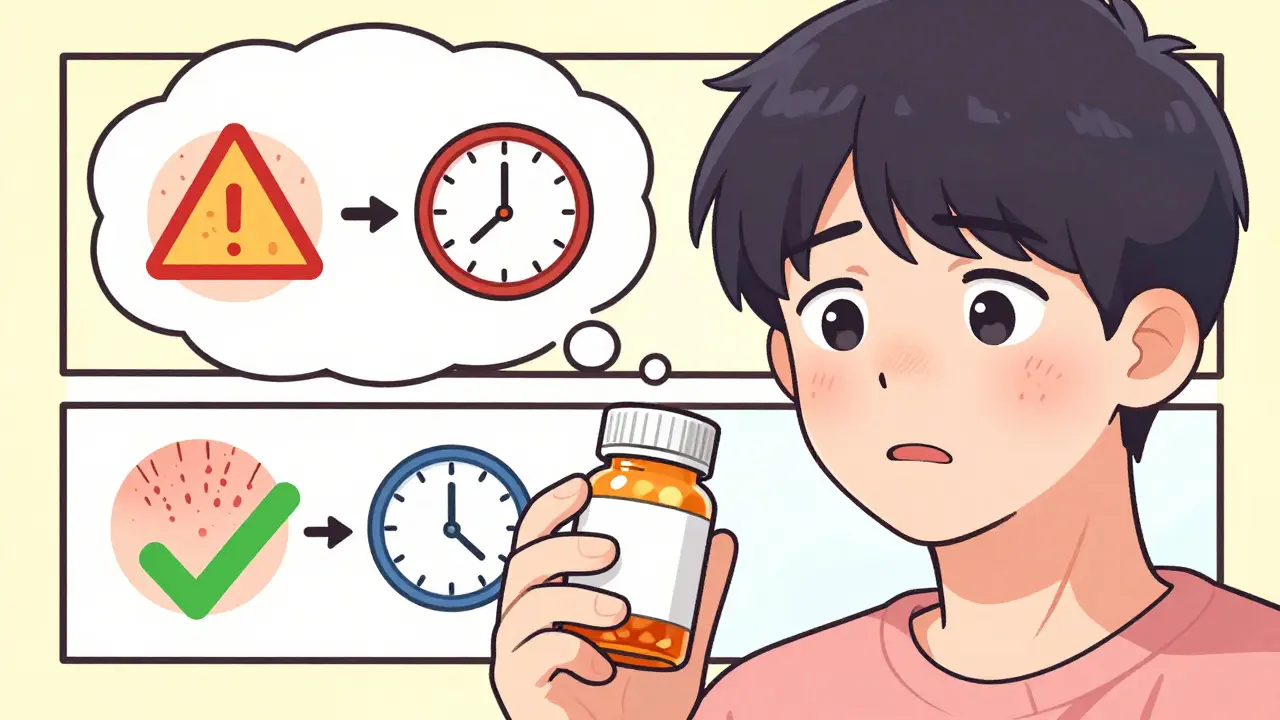
Timing Tells the Story
One of the clearest ways to tell the difference is when the reaction happens.
If you get hives, swelling, or feel dizzy within minutes to an hour after taking a pill - especially with a drug like penicillin - that’s a red flag for an IgE-mediated allergy. These reactions can escalate fast. Anaphylaxis usually hits within 10 to 30 minutes. That’s not a side effect. That’s an emergency.
But if you started feeling nauseous 2 days after beginning an antibiotic? Or got a rash 10 days later? That’s trickier. Many delayed rashes - especially in kids on amoxicillin - are actually caused by a virus they already had, not the drug. Doctors call this a "viral exanthem." But too often, it gets labeled as a "penicillin allergy," and that label sticks for life.
Side effects like dry cough from ACE inhibitors or frequent urination from SGLT2 inhibitors? They show up within days and often get better over time. Allergies? They don’t fade with more exposure. They get worse.
The Real Cost of Getting It Wrong
Labeling a side effect as an allergy isn’t just a mistake - it’s dangerous.
Let’s say you’re told you’re allergic to penicillin. Even if you’re not. Now, when you get a serious infection like pneumonia or a UTI, your doctor can’t use the most effective, safest, cheapest antibiotic. Instead, they have to pick something broader - like vancomycin or ciprofloxacin. Those drugs are more expensive. They’re harder on your gut. And they increase your risk of getting a deadly infection called Clostridioides difficile - by 2.5 times.
Studies show patients wrongly labeled as penicillin-allergic pay over $1,000 more per hospital stay. In the U.S. alone, this mislabeling costs the system more than $1 billion a year. And it’s not just about money. It’s about access. People with fake "sulfa allergies" are denied effective treatments for UTIs. People told they’re allergic to NSAIDs miss out on pain relief that could help them move better and live longer.
Meanwhile, true allergies - the kind that cause anaphylaxis - are rare. Only 5 to 10% of all bad reactions are immune-driven. But because people confuse the two, doctors treat everyone like they’re at risk. That’s why you’ll see hospitals now running allergy de-labeling programs. They test people who say they’re allergic - and 90% of them turn out to be fine.
Penicillin: The Most Misunderstood Drug
Penicillin is the poster child for this problem. About 10% of Americans say they’re allergic. But when tested - with skin tests or supervised oral challenges - 95% of them can take it safely.
Why? Because many people had a reaction as a child. A rash. Maybe they had a virus at the same time. Or maybe the drug made them nauseous. They were told, "Don’t take penicillin again." And that’s all they ever heard.
But here’s the thing: penicillin allergies can fade. About 80% of people who had a true reaction in childhood lose their sensitivity within 10 years. If you were told you were allergic 20 years ago, you’re probably not anymore.
Testing is safe. It’s simple. A skin prick test takes 15 minutes. If it’s negative, you get a small oral dose under observation. If you’re cleared, you can go back to using the most effective antibiotics - without risk.
Side Effects: Annoying, But Not Dangerous
Let’s be clear: side effects aren’t harmless. Muscle pain from statins? Real. Diarrhea from metformin? Uncomfortable. Dizziness from blood pressure meds? Risky if you’re older.
But here’s the key: side effects can often be fixed. You don’t have to quit the drug. You can lower the dose. Take it with food. Add another medication to help - like an antihistamine for opioid-induced itching. Or switch to a similar drug in the same class.
Take ACE inhibitors. About 1 in 5 people get a dry cough. It’s not an allergy. It’s caused by bradykinin buildup. The solution? Switch to an ARB - a different type of blood pressure pill - and the cough goes away. No need to avoid the whole category.
Same with statins. If you get muscle aches, your doctor might try a different statin, reduce the dose, or add coenzyme Q10. You don’t need to stop all cholesterol meds. You just need the right adjustment.
True allergies? No adjustments. No workarounds. You have to avoid the drug - and often all drugs in that class. That’s why getting the diagnosis right matters so much.
What You Can Do Right Now
Don’t just accept a label. Ask questions.
- What exactly happened when you reacted? (Rash? Swelling? Vomiting? Trouble breathing?)
- When did it happen? (Within an hour? After 3 days? After a week?)
- Did you have a fever or feel sick with it? (That’s more likely a virus.)
- Did you get better after stopping the drug? Or did you need an epinephrine shot or steroids?
Write it down. Be specific. Don’t say, "I’m allergic to penicillin." Say, "I got a red, itchy rash 5 days after taking amoxicillin, but I didn’t have trouble breathing or swelling. I didn’t need epinephrine."
Then talk to your doctor. Ask: "Could this have been a side effect? Can we test me?"
Pharmacists are your allies too. Many hospitals now have allergy clinics staffed by allergists and pharmacists who specialize in this. If you’ve been told you’re allergic to something, ask if you can be evaluated. It’s free or low-cost in most cases. And it could change your life.

What Doctors and Hospitals Are Doing About It
More hospitals are waking up to this problem. In 2018, only 15% of U.S. hospitals had formal programs to check if people were truly allergic to penicillin. By 2023, that number jumped to 65%.
How? They’re using electronic health records to flag patients with vague allergy labels. Then they send them to allergy specialists. Pharmacists lead interviews. Skin tests are done. Oral challenges are supervised.
Results? In the Veterans Health Administration, pharmacist-led programs cut inappropriate penicillin avoidance by 80%. At Mayo Clinic, 85% of patients who thought they were allergic to penicillin passed a challenge test.
Even the FDA is stepping in. Starting in 2024, drug labels must include clearer guidance on how to distinguish allergies from side effects. Patient medication guides now include decision trees: "Did you have hives? Was it within an hour? Did you need emergency care?"
This isn’t just about medicine. It’s about safety. Mislabeling allergies leads to more antibiotic resistance, longer hospital stays, and higher death rates. Getting it right saves lives.
When to Worry - And When to Relax
Here’s a quick guide:
True Allergy Signs:
- Hives, swelling of lips/tongue/throat
- Wheezing, trouble breathing
- Drop in blood pressure, dizziness, fainting
- Anaphylaxis (requires epinephrine)
- Reaction happened within minutes to an hour
- Reaction happened every time you took the drug
Side Effect Signs:
- Nausea, vomiting, diarrhea
- Headache, dizziness, fatigue
- Muscle aches, skin rash (without swelling or breathing issues)
- Reaction started after a few days or weeks
- Reaction got better with time or dose change
- You had a virus or infection at the same time
If you’re unsure - don’t guess. Get it checked.
Can I outgrow a drug allergy?
Yes, especially with penicillin. About 80% of people who had a true allergic reaction as a child lose their sensitivity within 10 years. Even if you had a severe reaction, it doesn’t mean you’ll always react. Testing can confirm whether you’re still allergic.
Is a rash always a sign of drug allergy?
No. Many rashes - especially in children - happen while they’re sick with a virus. Amoxicillin is often blamed, but it’s the virus causing the rash, not the drug. This is called a viral exanthem. It’s not an allergy. But without testing, it’s often mislabeled.
Can I take a different antibiotic if I’m allergic to penicillin?
Maybe - but not always. If you have a true penicillin allergy, you should avoid all penicillin-type drugs (like amoxicillin). But many people labeled as allergic can safely take them. If you’re unsure, get tested. You might not need to avoid other classes like cephalosporins, which are often just as effective.
How is a drug allergy diagnosed?
For penicillin, skin testing is the gold standard. A small amount of the drug is placed under the skin. If there’s no reaction, you may get a small oral dose under supervision. For other drugs, doctors use a graded oral challenge - slowly increasing the dose while watching for symptoms. Blood tests are less reliable and rarely used.
What if I had a severe reaction years ago? Should I still avoid the drug?
If you had a true anaphylactic reaction, you should still avoid the drug - unless you’ve been tested and cleared. But if you only had a rash or stomach upset, it’s likely not a true allergy. Talk to an allergist. Don’t assume you’re still allergic. Many people live with unnecessary restrictions for decades.
Can I be allergic to a drug I’ve taken before without problems?
Yes. Allergies can develop after repeated exposure. Your immune system can suddenly start recognizing a drug as harmful. That’s why even if you took penicillin safely in the past, you can still develop an allergy later. But if you’ve taken it multiple times without issue, you’re very unlikely to suddenly become allergic.

Fabian Riewe
December 29, 2025 AT 13:32Finally, someone put this into plain terms. I had a rash after amoxicillin as a kid and was labeled allergic for 25 years. Got tested last year-turned out I was fine. Now I can take penicillin for infections without worrying about $1,000+ bills. This article saved me years of unnecessary stress.
Paige Shipe
December 31, 2025 AT 02:56While I appreciate the intent behind this piece, I must point out that the conflation of side effects with allergies is not merely a diagnostic oversight-it is a systemic failure rooted in inadequate physician training and lazy documentation practices. The medical community must adopt standardized nomenclature and mandatory re-evaluation protocols for all allergy labels older than five years. Otherwise, we continue to perpetuate preventable harm.
David Chase
January 1, 2026 AT 19:52OMG YES!!! 😤 I’ve been saying this for YEARS!! My sister got a rash on amoxicillin and now she can’t get ANY antibiotic for UTIs-so they give her cipro and she gets C. diff. Like, wtf?? This is why America’s healthcare is broken. We’re treating people like walking allergies instead of actual humans. 🤦♂️ #PenicillinMyth #StopTheMadness
Emma Duquemin
January 2, 2026 AT 04:04Oh my goodness, this is the most important public health message I’ve read in years. I work in urgent care and see this every single day-patients who’ve avoided life-saving meds for decades because someone told them they were ‘allergic’ after a stomachache at age 7. One woman cried when she found out she could safely take penicillin again after 30 years. We’re not just saving money-we’re saving lives, dignity, and peace of mind. Thank you for writing this. Please share it everywhere.
Kevin Lopez
January 3, 2026 AT 12:21Non-IgE mediated reactions ≠ allergies. Misclassification rate: >90%. Penicillin de-labeling protocols reduce antibiotic resistance by 22%. C. diff risk drops 40%. Cost savings: $1.2B/year. Data is clear. Action is overdue.
Samar Khan
January 4, 2026 AT 08:30Bro I had the same thing 😭 I took amoxicillin for a sore throat when I was 8, got a rash, and now I’m 32 and they still won’t give me anything normal. I had to pay $300 to get tested. Worth every penny. Now I can take penicillin again. Why isn’t this routine??
Russell Thomas
January 5, 2026 AT 18:34So let me get this straight-you’re telling me I’ve been avoiding penicillin since 2005 because I got a rash while I had mono… and that’s not even a real allergy? And now you want me to trust a skin test? What’s next? Asking me to believe in astrology?
Joe Kwon
January 6, 2026 AT 05:08Great breakdown. I’m an ER pharmacist and we’ve started running allergy clarification clinics. Most patients are shocked when they find out they’re not allergic. The key is timing + symptoms. Hives + breathing issues = true allergy. Rash + fever + no swelling = likely viral. We’re seeing real change-patients are walking out with better options, not just fear.
Nicole K.
January 7, 2026 AT 13:37This is dangerous misinformation. If you got sick from a drug once, you should never take it again. Your body knows what it doesn’t like. Why risk it? People die from allergies. Don’t play doctor.
Tamar Dunlop
January 7, 2026 AT 20:16It is with profound solemnity that I acknowledge the gravity of this discourse. In my homeland of Canada, where healthcare is a sacred covenant between citizen and state, the persistence of mislabeled drug allergies constitutes not merely a clinical error-but a moral failing. To deny a patient access to the most efficacious, least toxic therapeutic agent due to outdated, unverified nomenclature is to betray the very ethos of evidence-based medicine. I implore all medical institutions to adopt mandatory re-evaluation protocols, and to empower pharmacists as frontline arbiters of truth. The lives of our mothers, fathers, children-depend upon it.
Amy Cannon
January 8, 2026 AT 02:52So I just want to say-this is the most important thing I’ve read all year. I’m a nurse, and I’ve seen patients get stuck with vancomycin because they were told they were allergic to penicillin when they were 4 and had a rash from a virus. And then they get C. diff and spend weeks in the hospital. And the worst part? No one ever asked them to describe what actually happened. It’s just written down as ‘penicillin allergy’ and that’s it. Forever. I’m going to start asking my patients: ‘What did it look like? When did it happen? Did you feel like you were dying?’ Because if not-that’s not an allergy. That’s a mistake. And we can fix it.
Himanshu Singh
January 8, 2026 AT 12:06Wow this is life changing! I thought I was allergic to sulfa because I got a rash once. Now I know it was probably the flu. I’m gonna ask my doc about testing. Thank you so much for sharing this. 🙏