Weight Loss Estimator Calculator
How Much Weight Can You Lose?
Based on clinical trial data for GLP-1 agonists like semaglutide and tirzepatide
For years, weight loss was seen as a matter of willpower: eat less, move more. But for millions of people struggling with obesity, that advice didn’t work - not because they weren’t trying, but because biology fights back. Now, a new class of medications originally designed for diabetes is reshaping how we think about weight, health, and long-term metabolic recovery. These are the GLP-1 agonists, and they’re doing more than lowering blood sugar. They’re changing how hunger works.
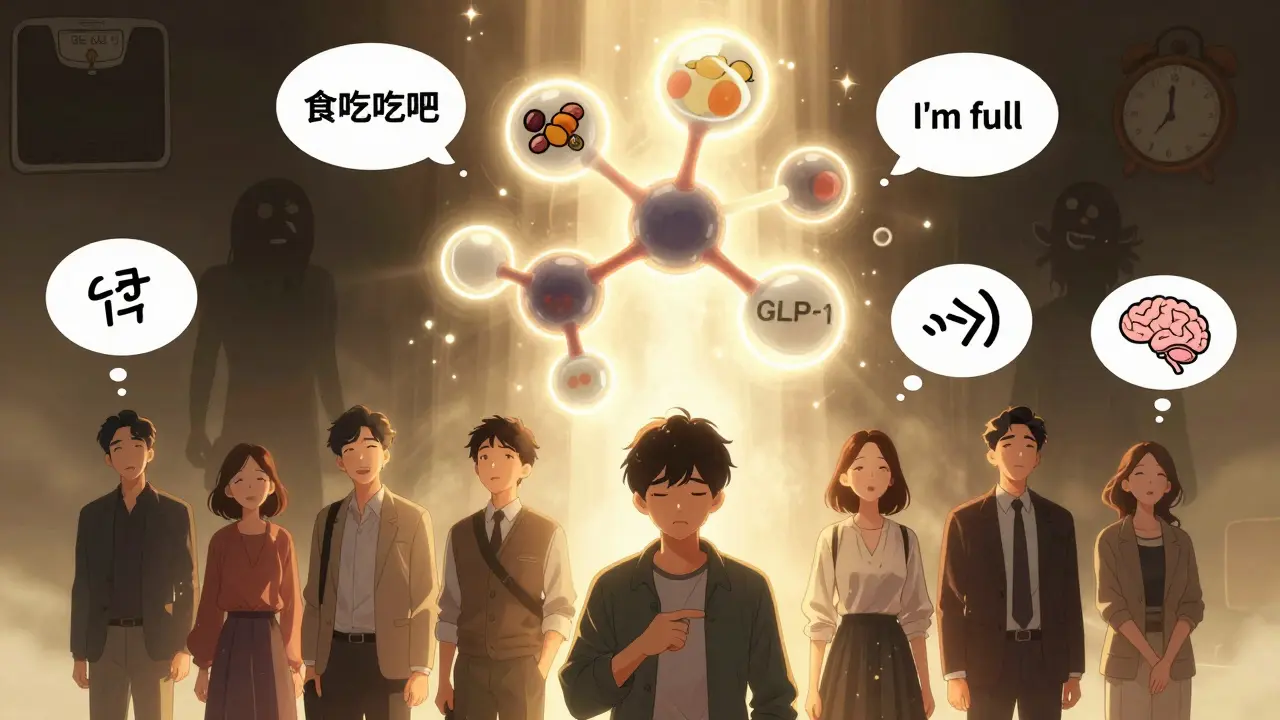
How GLP-1 Agonists Actually Work
GLP-1 stands for glucagon-like peptide-1. It’s a hormone your gut makes after you eat. It tells your pancreas to release insulin - but only when blood sugar is high. That’s smart design: no dangerous drops in blood sugar. It also slows down how fast food leaves your stomach, so you feel full longer. And here’s the key part: it sends signals to your brain that reduce appetite. You don’t just eat less because you’re trying to. You eat less because your brain doesn’t want to eat as much.
GLP-1 agonists like semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound) mimic this natural hormone. They’re not appetite suppressants like old diet pills. They don’t make you jittery or anxious. Instead, they work with your body’s own systems. Studies show they reduce cravings, especially for high-fat, high-sugar foods. People on these drugs often say they no longer feel obsessed with food. It’s not magic - it’s biology being reset.
Weight Loss Numbers You Can’t Ignore
Let’s talk numbers - real ones from real studies. In the STEP-1 trial, people using semaglutide 2.4 mg weekly lost an average of 14.9% of their body weight over 68 weeks. That’s not a few pounds. For someone weighing 200 pounds, that’s nearly 30 pounds gone. Compare that to lifestyle changes alone - the placebo group lost just 2.4%. The difference isn’t subtle. It’s life-changing.
Tirzepatide, a newer dual-acting drug that also mimics GIP (another gut hormone), pushes those numbers even higher. In trials, people on the highest dose (15 mg weekly) lost over 20% of their body weight. That’s more than one-fifth of their starting weight. About 60% of those participants hit that 20% mark. This isn’t an outlier. It’s repeatable.
Even older GLP-1 drugs like liraglutide (Saxenda) and dulaglutide (Trulicity) deliver 5-10% weight loss on average. That’s still more than most other treatments. And unlike insulin or sulfonylureas - which often cause weight gain - these drugs help you lose weight while keeping blood sugar stable.
Beyond the Scale: Heart, Brain, and Long-Term Health
The benefits don’t stop at the number on the scale. People taking GLP-1 agonists see real improvements in other areas of health:
- Heart health: Studies show a 12-18% lower risk of major heart events like heart attack or stroke, especially in people with existing heart disease or high risk.
- Blood pressure: On average, systolic pressure drops by 5-7 mmHg - similar to what you’d see with blood pressure meds.
- Cholesterol: LDL (bad cholesterol) goes down, HDL (good cholesterol) goes up.
- Brain function: A 2024 study of 2 million U.S. veterans found users had 23% fewer seizures, 17% lower risk of substance use disorders, and 14% less suicidal ideation than those on other diabetes drugs.
- Metabolic health: Fatty liver disease (NAFLD) improves. Inflammation markers like CRP drop. Insulin sensitivity gets better.
This isn’t just weight loss. It’s metabolic healing. That’s why the American Diabetes Association now recommends GLP-1 agonists as a first-line treatment for type 2 diabetes - especially if you also have obesity or heart disease.

Who Benefits Most - And Who Doesn’t
These drugs aren’t for everyone. They work best in people with:
- Type 2 diabetes
- Obesity (BMI ≥30, or ≥27 with weight-related conditions)
- Prediabetes
- Cardiovascular disease
But if you’re lean, have no metabolic issues, and just want to lose 5 pounds? The risk-benefit ratio doesn’t make sense. Side effects like nausea and vomiting are common - especially early on - and they’re not worth it for minor weight loss.
Also, don’t expect miracles if you’re not making lifestyle changes. These drugs don’t replace healthy eating or movement. They make it easier. People who combine the medication with nutrition counseling and regular activity lose more, keep it off longer, and report better quality of life.
The Side Effects: Real Talk
Yes, there are downsides. About 30-50% of people experience gastrointestinal issues: nausea, vomiting, diarrhea, constipation. For most, these fade after a few weeks. But for some, they stick around. One Reddit user wrote: “Constant nausea made it hard to focus at work. I had to drop the dose.”
Another concern is “Ozempic face” - a term used online to describe facial fat loss that can make some people look older or gaunt. While not medically recognized as a side effect, dermatologists are seeing it in long-term users. It’s likely related to overall fat loss, not just facial fat. It’s not dangerous, but it’s noticeable.
There’s also a small risk of pancreatitis (0.5-1% of users) and gallbladder problems. These are rare, but they’re real. That’s why these drugs require a doctor’s supervision. Never self-prescribe or buy from unregulated sources.

Cost and Access: The Biggest Barrier
As of early 2026, Wegovy costs about $1,349 per month without insurance. Zepbound is similar. That’s out of reach for most people. Even with insurance, many plans require prior authorization or only cover it for diabetes - not weight loss. In 2023, 60% of semaglutide prescriptions were for weight loss, but only 2% of eligible people actually got the drug.
Some companies are starting to cover it. Amazon, Walmart, and other big employers added GLP-1 agonists to their health plans in 2024. Manufacturer assistance programs help - Novo Nordisk covers up to 75% of out-of-pocket costs for eligible Wegovy users. Telehealth services like Found and Calibrate bundle the drug with coaching, but they cost $99-$149/month on top of the medication.
Supply shortages have improved since 2023, but demand still outpaces production. If you’re starting now, expect delays.
What Happens When You Stop?
This is the hardest part. If you stop taking the drug, you’ll likely regain weight. Clinical trials show 50-70% of lost weight comes back within a year of stopping. That doesn’t mean the drug failed. It means obesity is a chronic condition - like high blood pressure or asthma. You don’t stop taking your blood pressure meds just because your pressure is normal. You keep managing it.
Some people transition to lower doses. Others combine the drug with long-term behavioral support. A few find their metabolism resets enough to maintain weight without medication. But for most, it’s a long-term tool, not a quick fix.
What’s Next?
Researchers are working on next-gen versions:
- Oral pills with better absorption (Novo Nordisk’s 50 mg oral semaglutide is in Phase 3 trials)
- Implants that last 6-12 months
- Triple agonists that mimic GLP-1, GIP, and glucagon at once
- Combination therapies with amylin analogs
Market analysts predict global sales will hit $100 billion by 2030. That’s not just about weight loss - it’s about preventing heart disease, diabetes, liver disease, and even neurological conditions.
The biggest question isn’t whether these drugs work. It’s whether healthcare systems can afford to make them accessible. And whether we’ll treat obesity as a medical condition - not a moral failing.
Are GLP-1 agonists only for people with diabetes?
No. While they were first approved for type 2 diabetes, drugs like Wegovy and Zepbound are now FDA-approved specifically for chronic weight management in adults with obesity or overweight (with at least one weight-related condition). Many people without diabetes use them for weight loss, and this is now the most common reason for prescriptions.
How long does it take to see weight loss results?
Most people start noticing reduced appetite and slight weight loss within the first 2-4 weeks. Significant weight loss - 5% or more of body weight - typically happens by weeks 12-16. Maximum results usually occur around 6-12 months, depending on the dose and individual response.
Can I take GLP-1 agonists if I have a history of thyroid cancer?
No. GLP-1 agonists carry a boxed warning for thyroid C-cell tumors in rodents. While there’s no proven risk in humans, they are contraindicated in people with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Always discuss your full medical history with your doctor before starting.
Do I need to inject these drugs?
Most are injected once weekly (semaglutide, tirzepatide, liraglutide). But there’s an exception: oral semaglutide (Rybelsus) is taken daily as a pill. It’s less potent than the injectable versions and is only approved for diabetes, not weight loss. Injectable forms remain the gold standard for weight management.
Is it safe to use GLP-1 agonists long-term?
Current data shows they’re safe for long-term use in people who need them. Studies have followed users for up to 4 years with no new safety signals beyond known side effects. The biggest concern isn’t the drug itself - it’s whether people can maintain healthy habits after stopping. Long-term use may be necessary for sustained weight control, similar to how blood pressure or cholesterol meds are used.
Can I drink alcohol while taking GLP-1 agonists?
Moderate alcohol is generally okay, but it can increase the risk of low blood sugar (hypoglycemia), especially if you have diabetes. Alcohol also worsens nausea and can trigger vomiting. Many users report reduced interest in alcohol while on these drugs - which may be a benefit for those with unhealthy drinking patterns.