Fentanyl Patch Heat Exposure Calculator
Heat Exposure Safety Calculator
Calculate if your current heat exposure is safe while using a fentanyl patch based on article research
It’s not just about taking the patch. It’s about what’s around it. If you’re using a fentanyl patch for chronic pain, you might think the biggest danger is taking too many pills or mixing it with alcohol. But here’s something many people don’t know: heat can turn a safe, controlled dose into a life-threatening overdose - even if you haven’t touched the patch since you put it on.
How Fentanyl Patches Work (And Why Heat Changes Everything)
Fentanyl patches, like Duragesic, are designed to release a steady, low dose of opioid painkiller through your skin over three days. The patch isn’t just a sticky bandage - it’s a tiny drug delivery system. Inside, fentanyl is stored in a gel or reservoir, and it slowly moves through micropores in the patch, then through your skin, into your blood vessels, and finally to your brain. This process takes time. It can take up to 72 hours to reach a steady level in your blood, and that’s the whole point: consistent pain control without spikes.
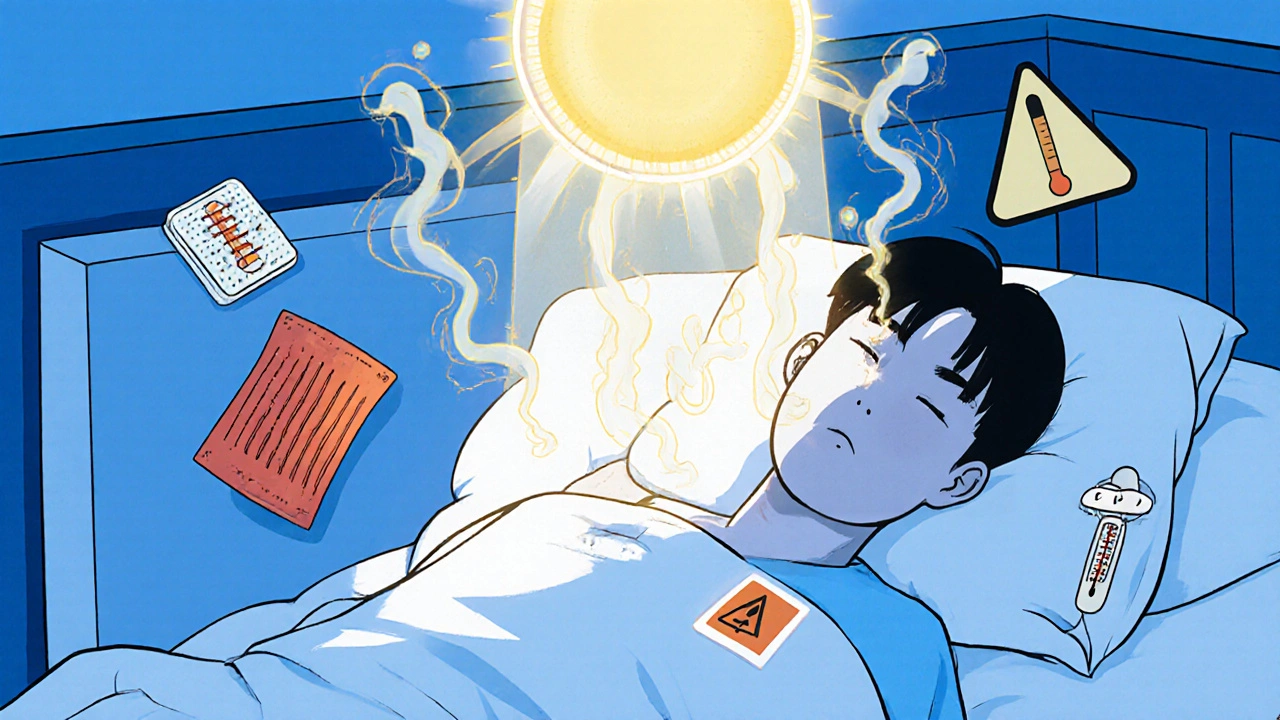
But heat changes the math. When your skin gets warm - whether from a heating pad, a hot shower, a fever, or even intense exercise - your blood vessels near the surface expand. More blood flows to the area under the patch. The fentanyl doesn’t wait to trickle out anymore. It rushes through. Studies show that when skin temperature hits 40°C (104°F), fentanyl absorption can jump by 33%. In one controlled experiment, researchers used a special heat patch over a fentanyl patch and saw serum levels rise nearly three times higher than normal.
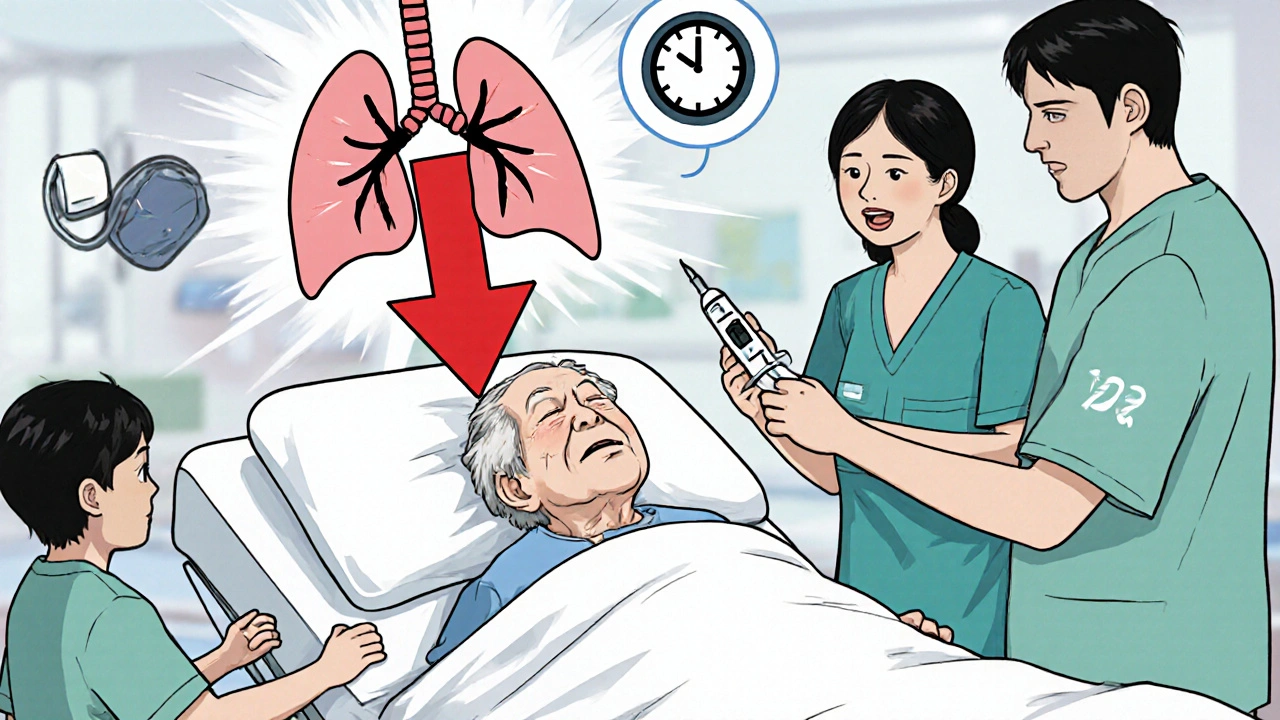
Real Cases: Heat Turned a Patch Into a Killer
This isn’t theoretical. The Medical Letter documented three real cases where heat exposure led to respiratory failure:
- A patient using a heating pad for back pain - collapsed with slowed breathing.
- A cancer patient in surgery - given a warming blanket to prevent hypothermia - stopped breathing and died.
- An elderly man who took a long, hot bath - developed extreme drowsiness and needed emergency reversal.
In each case, the patient was taking the patch exactly as prescribed. No extra doses. No mixing drugs. Just heat. And that was enough.
What Counts as Heat? (It’s More Than You Think)
Most people know not to use a heating pad. But the risks go deeper:
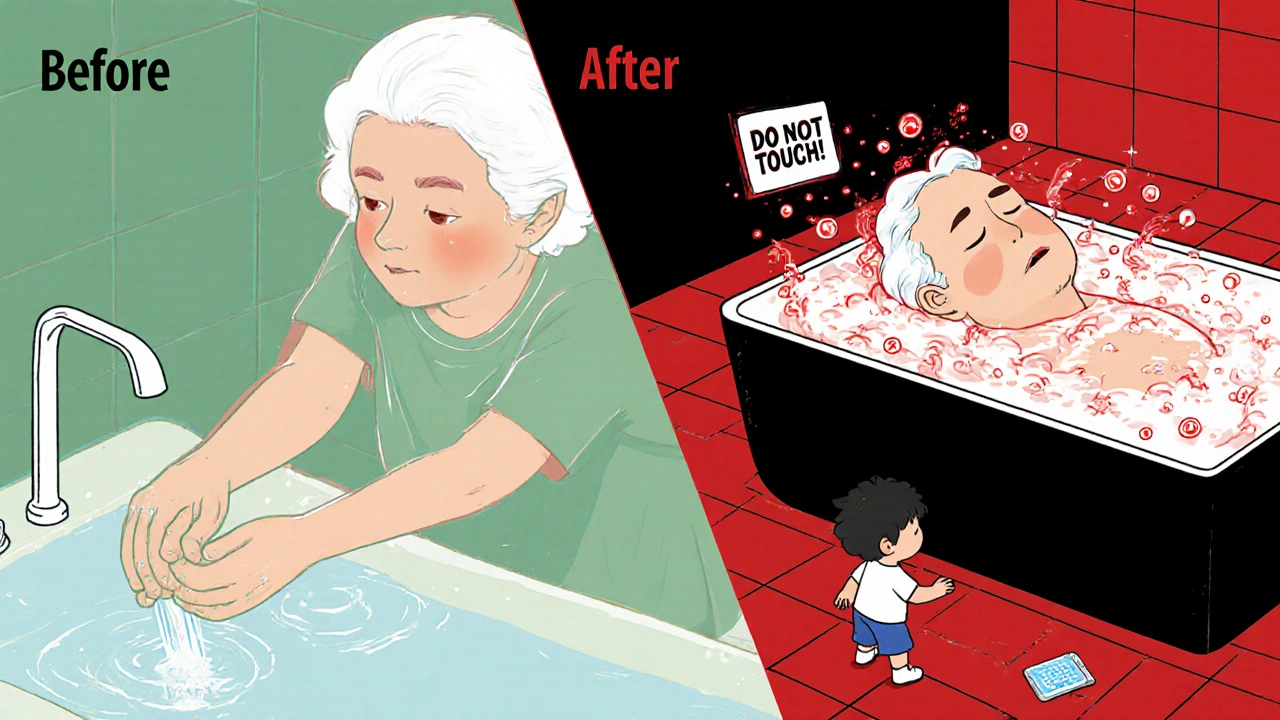
- Hot showers or baths - Water over 105°F (40.5°C) can trigger dangerous absorption.
- Saunas and steam rooms - High heat + humidity = double risk.
- Sunbathing - Lying in direct sun for hours warms your skin significantly.
- Electric blankets - Even on low, they can raise skin temperature over hours.
- Heated car seats - Especially dangerous if you sit for long drives.
- Fever - A temperature of 101°F or higher can increase absorption. Don’t ignore a fever if you’re on a patch.
- Exercise - Heavy lifting, gardening, or even brisk walking in warm weather can raise core temperature enough to matter.
And here’s the scary part: even after you remove the patch, fentanyl is still in your skin and fat tissue. It keeps releasing for hours - sometimes up to 24 hours. So if you take a hot shower the next day after removing the patch, you’re still at risk.
Who’s Most at Risk?
Fentanyl patches are not for everyone. They’re only approved for people who are already tolerant to opioids - meaning they’ve been taking strong painkillers regularly for weeks or months. If you’ve never taken opioids before, even one patch can kill you. That’s why they’re never used for acute pain, like after surgery.
But even among those who are tolerant, some groups are more vulnerable:
- Older adults - Slower metabolism means fentanyl stays in the body longer.
- People with liver or kidney problems - Their bodies clear fentanyl slower.
- Those taking other medications - Drugs like ketoconazole, erythromycin, or even some antidepressants can block the liver enzymes that break down fentanyl, causing levels to spike.
- People with chronic illnesses - Cancer patients, for example, often have fevers or are bedridden under warming blankets.
What You Must Do - And What You Must Avoid
If you or someone you care for is using a fentanyl patch, here’s your non-negotiable checklist:
- Never use a heating pad, electric blanket, or heated mattress.
- Avoid saunas, hot tubs, and long hot showers or baths.
- Stay out of direct sun for long periods - wear loose, light clothing.
- Monitor your temperature - If you get a fever (100.4°F or higher), call your doctor immediately. Don’t wait.
- Limit intense activity - Avoid heavy lifting, vigorous exercise, or working in hot environments.
- Check all your medications - Tell your pharmacist and doctor you’re on a fentanyl patch. They need to screen for drug interactions.
- Remove the patch after exactly 72 hours - Don’t leave it on longer. Don’t cut it. Don’t fold it.
- Dispose of used patches safely - Fold the sticky side inward, flush it down the toilet, or take it to a drug take-back program. Kids or pets can overdose just by touching a used patch.
Symptoms of Overdose - Don’t Wait
Signs of too much fentanyl don’t always look like the movies. It’s not always unconsciousness. Early warning signs include:
- Extreme drowsiness or confusion
- Slow, shallow, or irregular breathing
- Pinpoint pupils
- Cold, clammy skin
- Dizziness or fainting
- Unresponsiveness
If you see any of these, call emergency services right away. If you have naloxone (Narcan) on hand, use it. It won’t hurt - and it might save a life. Naloxone reverses opioid overdose, even from patches.
What Your Doctor Should Be Asking You
Too often, patients are given the patch and sent home with a pamphlet. That’s not enough. Your doctor should ask:
- Do you have a fever or get hot easily?
- Do you use heating pads or electric blankets?
- Do you take hot baths or showers regularly?
- Are you on any other medications - even over-the-counter ones?
- Have you had any recent changes in your activity level?
If your doctor doesn’t ask these questions, ask them yourself. This isn’t about being difficult. It’s about staying alive.
The Bigger Picture
Fentanyl patches are a lifeline for people with severe, chronic pain - especially those with cancer or advanced arthritis. They offer steady relief without swallowing pills every few hours. But that convenience comes with a hidden danger. Heat is silent. It doesn’t come with a warning label you can see. It doesn’t make noise. It just warms your skin - and changes how your body handles a powerful drug.
Regulators know this. The FDA, Mayo Clinic, and medical journals have all issued clear warnings. But awareness hasn’t caught up with the risk. Too many people still think, ‘I’m not doing anything wrong - I’m just taking my patch.’
Heat isn’t just a nuisance. It’s a multiplier. And in the case of fentanyl, multipliers can be deadly.
Can I use a fentanyl patch if I have a fever?
No. A fever raises your body temperature, which increases how fast fentanyl is absorbed through your skin. This can lead to dangerous blood levels and overdose. If you develop a fever while using a fentanyl patch, contact your doctor immediately. Do not wait for symptoms to appear.
Is it safe to take a warm shower with a fentanyl patch?
It’s not recommended. Water hotter than 105°F (40.5°C) can significantly increase fentanyl absorption. If you must shower, keep it short and use lukewarm water. Avoid soaking in a hot tub or bath. Even after removing the patch, residual fentanyl can still be absorbed for up to 24 hours - so the risk doesn’t disappear.
Can I exercise while wearing a fentanyl patch?
Light activity like walking is usually okay. But avoid strenuous exercise - especially in hot weather. Heavy lifting, running, or working outdoors can raise your core temperature and trigger faster drug absorption. If you feel dizzy, short of breath, or unusually sleepy during activity, stop immediately and seek help.
What should I do if I accidentally expose my patch to heat?
Remove the patch immediately. Call your doctor or go to the nearest emergency room. Do not wait for symptoms. Even if you feel fine, fentanyl levels may still be rising. If you have naloxone available, keep it nearby. Overdose can happen suddenly and without warning.
Are there safer alternatives to fentanyl patches?
Yes. For chronic pain, alternatives include long-acting oral opioids (like extended-release oxycodone), non-opioid pain relievers (like gabapentin or duloxetine), nerve blocks, or physical therapy. If you’re concerned about heat risks, talk to your doctor about switching to a delivery method that doesn’t rely on skin absorption. Your pain management plan should be personalized - not just prescribed.
Can I use a fentanyl patch after surgery?
No. Fentanyl patches are not approved for acute pain, including post-surgery pain. They’re only for patients already tolerant to opioids. Using them after surgery - especially in opioid-naïve people - can cause fatal respiratory depression. Always tell your surgical team if you’re using a fentanyl patch before any procedure.

Robert Bashaw
November 29, 2025 AT 18:17Okay so let me get this straight - you’re telling me that just taking a hot shower could turn my pain patch into a silent killer? 🤯 I thought the worst part was forgetting to wash my hands after changing it. Now I’m scared to sweat, to cuddle my dog under the blanket, or even walk to my damn mailbox in summer. This isn’t medicine - it’s a Russian roulette with a heat gun. 😭
Subhash Singh
December 1, 2025 AT 07:02It is imperative to underscore the pharmacokinetic implications of elevated dermal temperature on transdermal fentanyl absorption. The increased cutaneous blood flow, coupled with enhanced diffusion gradients, leads to a non-linear escalation in plasma concentration. This phenomenon, well-documented in peer-reviewed literature, necessitates stringent patient education and clinical vigilance, particularly in geriatric and polypharmacological populations.
Geoff Heredia
December 1, 2025 AT 14:34They don’t want you to know this - but the FDA, Big Pharma, and your doctor are all in on it. Heat? That’s just the cover. The real danger? The patch is designed to slowly poison you so you stay dependent. They don’t want you cured - they want you warm, drowsy, and buying new patches every 3 days. And don’t get me started on the ‘flush it down the toilet’ advice… that’s how they’re poisoning the water supply. 🕵️♂️💧
Tina Dinh
December 2, 2025 AT 02:12Y’all. I’m so glad this was posted. My dad’s on these patches and I’ve been begging him to stop using his heated blanket. 😭 I literally cried when I read this. Please, if you’re using one - tell someone. Share this. I don’t want anyone to lose someone because they didn’t know. 💕❤️🫂
Andrew Keh
December 3, 2025 AT 06:47This is important information that should be shared more widely. Many people assume that if they follow the prescription, they’re safe. But heat is an invisible risk. Simple steps like avoiding hot baths and checking for fever can make a big difference. Thanks for bringing this up.
Peter Lubem Ause
December 4, 2025 AT 09:55Let me tell you something - this isn’t just about patches. This is about how we treat chronic pain in this country. We hand out opioids like candy and then act shocked when people get hurt. The real problem? No one checks in. No one asks if you’re too hot. No one says, ‘Hey, did you take a sauna this week?’ You get a patch, a pamphlet, and a prayer. That’s not care. That’s negligence dressed in white coats. But here’s the good part - you can change it. Talk to your doctor. Ask the questions. Demand better. You’re not being difficult - you’re being alive.
linda wood
December 6, 2025 AT 08:39So let me get this straight - I’m supposed to be warm enough to feel pain relief but not warm enough to die? That’s like being told to breathe but not inhale. 😒 And who decided ‘lukewarm’ means 105°F? That’s a damn Jacuzzi. Also, why does no one ever tell you that the patch still leaks poison for a whole day after you peel it off? That’s not a warning - that’s a trap.
LINDA PUSPITASARI
December 8, 2025 AT 08:12I work in hospice and this is SO real. We had a patient last month who just took a long shower after patch change and coded. He was so sweet. Just wanted to feel clean. No one told him about the heat risk. We’ve started putting little sticky notes on the patches now - ‘NO HOT WATER’ - and it’s made a difference. Please share this. Someone’s grandma might be reading this right now. 🙏❤️
gerardo beaudoin
December 9, 2025 AT 00:17Man I never knew this. I’ve been using my heating pad for years with my patch. I’m gonna stop today. No excuses. This is scary but also super helpful. Thanks for sharing.
Joy Aniekwe
December 9, 2025 AT 13:40Oh wow, so now I’m supposed to feel guilty for wanting to be warm? Because apparently, chronic pain patients are just walking toxicity bombs who can’t even enjoy a bath without becoming a public health hazard. How convenient. Let’s blame the victim instead of fixing the system. 🙄
Latika Gupta
December 10, 2025 AT 21:23Can I ask - do you know if this applies to infrared heating lamps? I’ve been using one for my lower back and I’m not sure if it’s safe. I don’t want to risk anything. Thank you for your help.
Sullivan Lauer
December 11, 2025 AT 08:18Let me tell you something - I’ve been on these patches for five years. I’ve survived two heart attacks, a kidney transplant, and my ex-wife’s Christmas party. But this? This heat thing? This is the one thing that keeps me up at night. I don’t sleep with the AC on because I’m cold - I sleep with it on because I’m terrified of sweating in my sleep. I’ve stopped hugging my grandkids in winter because I don’t know if my body heat will push the patch over the edge. This isn’t just a warning - it’s a life sentence with no parole. And the worst part? No one talks about it. Not even my doctor. I had to Google it. I’m 68. I shouldn’t have to be a detective just to stay alive.
Sohini Majumder
December 12, 2025 AT 03:14OMG I can’t believe people still use these?? Like… are we living in the 1990s?? This is like giving someone a flamethrower and saying ‘be careful’… I mean, why not just inject heroin directly into your eyeball?? 🤦♀️ #FentanylIsTheNewCigarettes
tushar makwana
December 12, 2025 AT 18:01From India, I want to say thank you. In my country, many people don’t even know what a fentanyl patch is. Some use them like regular painkillers. I’ve seen people put them on their legs and sit in the sun all day. This post is a gift. Please share it in more languages. Someone’s mother is reading this right now, and she doesn’t know she’s in danger. You saved her life today.