HER2-positive breast cancer used to be one of the most aggressive types. About 1 in 5 women diagnosed with breast cancer have this subtype. Back in the 1990s, it meant a higher chance of recurrence and shorter survival. Today, that’s no longer the case. Thanks to targeted therapies, many patients now live longer, healthier lives-even with advanced disease. But what exactly are these treatments, and how do they actually work?
What Makes HER2-Positive Breast Cancer Different?
Not all breast cancers are the same. Some grow slowly. Others spread fast. HER2-positive breast cancer is driven by too much of a protein called HER2 on the surface of cancer cells. This protein acts like a switch, telling cells to grow and divide nonstop. When there’s too much HER2, tumors grow aggressively and are more likely to spread.
Doctors test for HER2 using a biopsy. Two common tests look at how much HER2 protein is present (IHC) and whether there are too many copies of the HER2 gene (FISH). If the results show HER2-positive, that means the cancer is fueled by this protein-and that opens the door to specific treatments designed to block it.
Before targeted therapies, treatment was mostly chemotherapy. It worked, but it hit healthy cells too, causing nausea, hair loss, and fatigue. Targeted therapies changed everything. They don’t just kill cells-they go after the exact mechanism driving the cancer.
The First Breakthrough: Trastuzumab and Its Biosimilars
Trastuzumab, sold as Herceptin, was the first drug approved to block HER2. It’s a monoclonal antibody, meaning it’s made in a lab to lock onto the HER2 protein like a key in a lock. Once attached, it stops the growth signal and tells the immune system to attack the cancer cell.
It’s given through an IV or, more recently, as a quick subcutaneous injection under the skin. The injection form, like Phesgo (which combines trastuzumab and pertuzumab), cuts treatment time from over an hour to under 10 minutes. Many patients say this change alone improved their quality of life.
Now, there are biosimilars-copies of trastuzumab that work the same way but cost less. Brands like Kanjinti, Ogivri, and Ontruzant are widely used. They’re not cheaper because they’re weaker. They’re cheaper because they don’t need the same research costs as the original.
Trastuzumab is often used with chemotherapy in early-stage cancer, given for a full year after surgery. For metastatic cancer, it’s used long-term. But it has limits. It doesn’t cross the blood-brain barrier well, so it’s less effective if the cancer spreads to the brain.
Dual Blockade: Adding Pertuzumab
Trastuzumab blocks one part of the HER2 signal. Pertuzumab (Perjeta) blocks another. Together, they shut down the HER2 pathway more completely. This combo, called dual blockade, became standard for larger tumors or high-risk early-stage cancer.
The KRISTINE trial showed that using both drugs before surgery (neoadjuvant therapy) led to higher rates of no remaining cancer cells after surgery. That’s a big deal-it means lower chances of the cancer coming back.
Phesgo, the fixed-dose combo of trastuzumab and pertuzumab with hyaluronidase, lets patients get both drugs in one subcutaneous shot. No more two separate IVs. No more sitting for 90 minutes. Just an 8-minute injection. For patients juggling work, kids, or travel, that’s life-changing.
Antibody-Drug Conjugates: The Next Leap
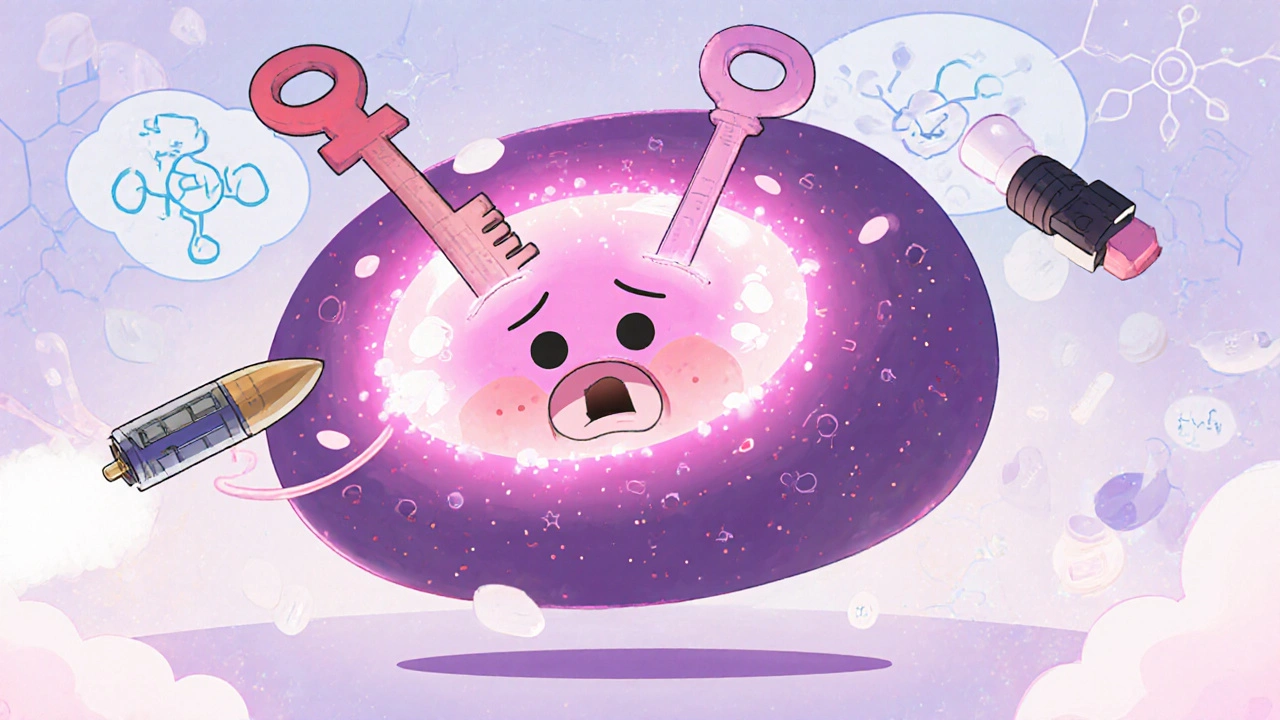
Then came antibody-drug conjugates (ADCs)-a new kind of targeted therapy. These drugs combine an antibody (to find the cancer cell) with a powerful poison (to kill it). The antibody delivers the poison directly, sparing healthy tissue.
T-DM1 (Kadcyla) was the first major ADC. It links trastuzumab to a chemo drug called emtansine. It’s used after trastuzumab and chemotherapy fail, especially in metastatic cases. It works better than chemo alone, but it’s not perfect. Side effects include low platelets and liver issues.
But the real game-changer is trastuzumab deruxtecan (T-DXd, brand name Enhertu). It’s not just a stronger poison-it’s designed to release its payload even into nearby cancer cells. That’s called the “bystander effect.”
The DESTINY-Breast03 trial showed T-DXd cut the risk of disease progression or death by 72% compared to T-DM1. Patients lived nearly twice as long without their cancer worsening. It’s now the go-to second-line treatment for metastatic HER2-positive breast cancer.
But T-DXd has a serious warning: interstitial lung disease. About 1 in 10 patients develop lung inflammation. It’s rare, but it can be life-threatening. Doctors monitor for cough or shortness of breath. Most cases are caught early and treated with steroids.
Tyrosine Kinase Inhibitors: Pills That Fight Brain Metastases
Not all HER2 drugs are injections. Some are pills-small molecule tyrosine kinase inhibitors (TKIs). They work inside the cell, blocking the HER2 signal at its source.
Lapatinib and neratinib were early options. But they caused severe diarrhea and rashes. Many patients couldn’t tolerate them.
Tucatinib (Tukysa) changed that. It’s more selective-it targets HER2 without hitting similar proteins that cause side effects. And crucially, it crosses the blood-brain barrier.
In the HER2CLIMB trial, adding tucatinib to trastuzumab and capecitabine improved survival in patients with brain metastases. Median survival jumped from 17.4 months to 21.9 months. That’s not just a statistic-it’s months of life with quality, with less fear of neurological decline.
Today, tucatinib is the first choice for HER2-positive breast cancer that has spread to the brain. It’s taken twice daily with food. Side effects include diarrhea and liver enzyme changes, but they’re usually manageable.
Cardiotoxicity: The Hidden Risk
Every HER2-targeted therapy has a trade-off. For trastuzumab and pertuzumab, it’s the heart. These drugs can weaken the heart muscle. About 2-7% of patients develop heart failure during treatment.
That’s why doctors check heart function before starting and every 3 months during therapy. An echocardiogram measures how well the heart pumps. If the number drops too low, treatment pauses or stops.
Patients often feel anxious about these tests. One woman on a support forum said, “I dread my echo appointment like a dentist visit. What if they say I have to stop?”
But the risk is real and manageable. Most heart issues reverse when treatment stops. Newer drugs like tucatinib and T-DXd have lower heart risks. Researchers are now testing heart-sparing combinations to make treatment safer long-term.
HER2-Low: A New Category, New Hope
Here’s something many don’t know: HER2-positive isn’t the only group that benefits from these drugs anymore.
Scientists now recognize “HER2-low” breast cancer-where HER2 is present but not enough to be called positive. About half of all breast cancers fall into this category. And T-DXd works here too.
The DESTINY-Breast04 trial showed T-DXd doubled progression-free survival compared to chemo in HER2-low metastatic cancer. That’s why ASCO guidelines now recommend it for this group.
This shift means more patients qualify for targeted therapy. What used to be a 15-20% group is now over 50%. And companies are rushing to develop more ADCs for HER2-low and even HER2-ultralow cancers.

What’s Next? The Future of HER2 Treatment
Over 150 clinical trials are active right now. New bispecific antibodies-drugs that bind to two targets at once-are showing promise. Zenocutuzumab and zanidatamab are in phase 3 trials, with early results showing response rates of 35-45% in heavily treated patients.
Researchers are also testing T-DXd with immunotherapy. Could combining a targeted drug with the immune system’s power make treatment even stronger? Trials like KEYNOTE-B48 are trying to find out.
And then there’s cost. T-DXd can run $17,000 a month in the U.S. Biosimilars help bring down trastuzumab prices, but ADCs remain expensive. Access isn’t equal. That’s a growing concern.
Still, the progress is undeniable. Where HER2-positive once meant a grim prognosis, it now often means long-term control-and sometimes, even cure.
Choosing the Right Treatment
There’s no one-size-fits-all. Your treatment depends on:
- Stage of cancer (early vs. metastatic)
- Whether it’s spread to the brain
- Your heart health
- Previous treatments
- Your tolerance for side effects
For early-stage: Trastuzumab + pertuzumab + chemo, followed by a year of trastuzumab.
For metastatic, first-line: Trastuzumab + pertuzumab + taxane chemotherapy.
For second-line: T-DM1 or T-DXd (if not used first).
For brain metastases: Tucatinib + trastuzumab + capecitabine.
For HER2-low: T-DXd is now standard after chemo.
Your oncologist will map out a plan based on your unique situation. It’s not about picking the “best” drug-it’s about picking the right one for you, right now.
Managing Side Effects: What Patients Need to Know
Each drug has its own side effect profile. Here’s what to watch for:
- Trastuzumab/pertuzumab: Heart issues, fatigue, fever, chills.
- T-DM1: Low platelets, liver enzyme spikes, nausea.
- T-DXd: Cough, shortness of breath (lung issues), nausea, fatigue.
- Tucatinib: Diarrhea (often mild), liver changes, hand-foot syndrome.
- Neratinib: Severe diarrhea-requires preventive loperamide.
Don’t wait until symptoms get bad. Tell your team early. Diarrhea can be controlled with loperamide. Lung symptoms need prompt imaging. Heart issues can be reversed if caught early.
Many patients say the biggest help is knowing what to expect. Ask for a written guide. Use apps to track side effects. Join a support group. You’re not alone.
Is HER2-positive breast cancer curable?
In early stages, yes-many patients are cured with surgery, chemotherapy, and a year of HER2-targeted therapy. In metastatic cases, it’s rarely curable, but it’s often controllable for years. With newer drugs like T-DXd and tucatinib, survival times have more than doubled over the past decade. Some patients live 5, 7, or even 10+ years with stable disease.
Can I get HER2-targeted therapy if I’ve had chemo before?
Absolutely. In fact, most HER2-targeted drugs are used after or alongside chemo. T-DM1 and T-DXd are specifically approved for patients who’ve already received trastuzumab and chemo. Tucatinib is used in later lines too. The sequence matters, but there are options even after multiple treatments.
Do I need genetic testing for HER2-targeted therapy?
You don’t need inherited gene testing like BRCA. You need a tumor test-HER2 IHC and FISH-to confirm the cancer overexpresses HER2. This is done on your biopsy sample. If it’s HER2-low, you may still qualify for T-DXd. The test doesn’t change over time, so it’s done once unless the cancer changes.
What if I develop heart problems during treatment?
If your heart function drops below a certain level, your oncologist will pause treatment. Most patients recover heart function with medications like ACE inhibitors or beta-blockers. Once your heart improves, some HER2 drugs can be restarted-though often at lower doses or with more frequent monitoring. Tucatinib and T-DXd carry lower heart risks, so they may be preferred if heart issues arise.
Are there cheaper alternatives to expensive drugs like T-DXd?
There are no biosimilars for T-DXd yet-it’s still under patent. But T-DM1 is cheaper and still effective for many. Clinical trials often offer access to new drugs at no cost. Patient assistance programs from drugmakers can reduce out-of-pocket costs. Talk to your oncology social worker-they help navigate financial support.
Can I take supplements or herbal remedies with HER2 therapy?
Some supplements can interfere with how these drugs work. Green tea extract, St. John’s wort, and high-dose antioxidants may reduce effectiveness or increase side effects. Always tell your oncologist what you’re taking-even if you think it’s “natural.” They can check for interactions. Safety first.
How often do I need scans during treatment?
For metastatic disease, scans (CT, MRI, or PET) are usually done every 2-3 months to check if the cancer is responding. If you’re on a stable treatment with no symptoms, scans might be spaced out. For early-stage, scans aren’t routine unless symptoms appear. The goal is to avoid unnecessary radiation while catching progression early.
Will I lose my hair with HER2-targeted therapy?
Not usually. Unlike chemo, drugs like trastuzumab, pertuzumab, T-DXd, and tucatinib don’t typically cause hair loss. You might notice thinning with T-DM1 or if you’re also getting chemo. Many patients appreciate that they can keep their hair-which helps with emotional well-being during treatment.
HER2-positive breast cancer is no longer a death sentence. It’s a chronic condition for many-and for others, a curable disease. The science behind these drugs is complex, but the outcome is simple: more time, more life, more hope. If you or someone you love has been diagnosed, ask about HER2 testing, ask about targeted options, and don’t settle for outdated answers. The treatment landscape has changed-and it’s changing faster than ever.

Nicole Ziegler
November 19, 2025 AT 13:51T-DXd changed my life. No hair loss, just mild nausea and I can still pick up my kids from school. 🙌
Summer Joy
November 21, 2025 AT 02:25Okay but can we talk about how T-DXd is basically a magic bullet? 😭 I mean, 72% reduction in progression?? And then they drop the lung disease bomb like it’s no big deal. Like… sure, 1 in 10 people get it, but what if you’re that one?? 🤯 #CancerIsNotATicketToTheMoon
Kristi Bennardo
November 21, 2025 AT 04:49This article is dangerously optimistic. The pharmaceutical industry is profiting off false hope. T-DXd costs $17,000 a month. Who exactly is this ‘hope’ for? The wealthy? The insured? The rest of us are just waiting to die while CEOs take vacations in Bali. 🤑
Bharat Alasandi
November 21, 2025 AT 21:31Man, tucatinib for brain mets is a game changer. My aunt was given 6 months, now she’s 3 years in and still driving. No hair, no chemo vibes, just pills and peace. 🙏
Aruna Urban Planner
November 22, 2025 AT 21:40The shift from HER2-positive to HER2-low as a therapeutic category represents a paradigmatic reconfiguration in oncologic taxonomy. The bystander effect of T-DXd, particularly in low-expression phenotypes, challenges the binary classification model and necessitates a re-evaluation of biomarker-driven therapeutic stratification. This is not merely incremental progress-it’s epistemic evolution.
Shiv Karan Singh
November 23, 2025 AT 07:55lol yeah right. 'Targeted therapy' my ass. They just found a new way to make people pay for poison. I bet 90% of these 'miracle drugs' are just repackaged chemo with a fancy name. And don't get me started on the heart risks. They'll kill you slow with one hand and sell you a heart monitor with the other. 💀
Ravi boy
November 24, 2025 AT 23:41i read this whole thing and im just like wow. my cousin had this and she did the trastuzumab shot and it was quick like 10 mins. she said she felt weird after but no hair loss so she was happy. also she ate a lot of ginger tea. idk if it helped but she lived
Matthew Peters
November 25, 2025 AT 01:14Wait… so T-DXd works on HER2-low too? That’s wild. So like… if you’re HER2-negative but borderline, you’re now eligible? That’s like the cancer version of ‘you’re not fat, you’re just big-boned.’ But in a good way. 🤯 This changes everything. I’m gonna send this to my sister who’s in remission. She’ll cry.
Matthew Karrs
November 25, 2025 AT 14:14Let’s be real. The whole HER2 narrative is a distraction. They’re not curing cancer. They’re just making it a longer, more expensive chronic illness. And those ‘clinical trials’? They’re just testing on desperate people. You think they care if you live 10 years? They care if you keep buying the next drug. The system is rigged. 🕵️♂️
Liam Strachan
November 25, 2025 AT 21:36Really appreciate this breakdown. I’ve got a friend on T-DXd and the lung monitoring part scared her-she didn’t know to watch for a dry cough. This helped her speak up to her doc. Thanks for the clarity. 🙏