Antibiotic Side Effect Manager
How to Manage Your Antibiotics
Enter your antibiotic details to get personalized side effect management strategies
Results
Key Management Tips
Common Side Effects to Watch For
Red Flags Requiring Medical Attention
Stopping your antibiotics early because of side effects might feel like the right thing to do-especially when you’re feeling sick from the medicine itself. But doing so can make your infection worse, increase your risk of needing stronger drugs later, and even contribute to antibiotic resistance. The truth is, most antibiotic side effects are manageable, and you don’t have to suffer through them alone. In fact, antibiotic side effects are so common that 1 in 5 people on antibiotics experience them. The good news? With the right strategies, you can finish your full course without quitting.
Most Antibiotic Side Effects Are Mild-and Normal
You’re not alone if you feel nauseous, get diarrhea, or lose your appetite while on antibiotics. These aren’t signs the drug is failing-they’re signs your gut microbiome is being disrupted. About 25% of people on antibiotics develop diarrhea. Nausea affects nearly 1 in 4, and bloating or loss of appetite is reported by 1 in 5. These symptoms usually start within a few days of beginning treatment and fade as your body adjusts. The key is knowing what’s normal versus what’s dangerous. Mild stomach upset, occasional loose stools, and reduced hunger are common. But if you develop bloody or mucus-filled diarrhea, severe abdominal cramps, fever, or vomiting that won’t stop, you could be dealing with a serious infection like C. diff. That needs immediate medical attention.Take Antibiotics the Right Way-Food Matters
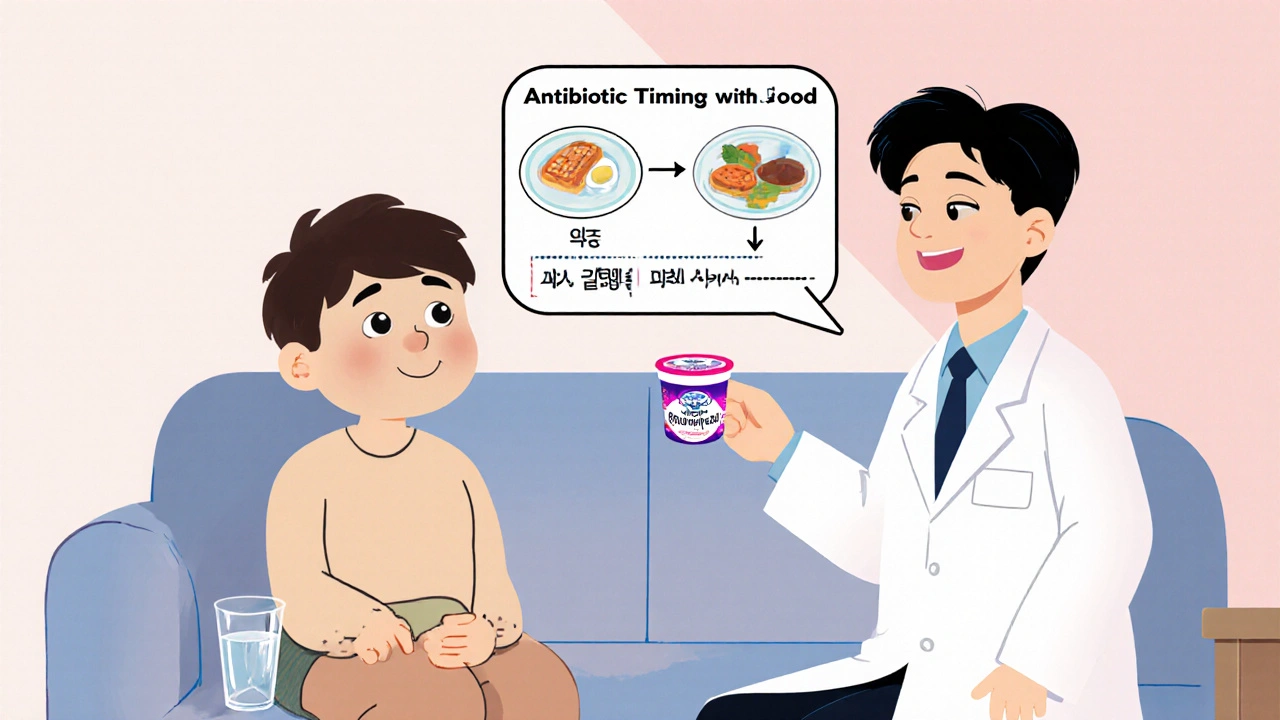
One of the simplest ways to reduce stomach upset is to take your antibiotic with food. But not all antibiotics work the same way. Some need to be taken on an empty stomach, others work better with food. Getting this wrong can make the drug less effective. - Take with food: Amoxicillin, azithromycin, doxycycline (unless your doctor says otherwise), and cephalexin. A small snack like crackers, toast, or Greek yogurt helps buffer your stomach. Avoid heavy, greasy meals-they can make nausea worse. - Take on an empty stomach: Tetracycline, doxycycline (if prescribed for acne or certain infections), and minocycline. These drugs bind to calcium, iron, and dairy, which blocks absorption. Wait at least 1 hour before or 2 hours after eating. - Drink plenty of water: Especially with doxycycline. Swallow it with a full glass of water while sitting upright. Lying down right after can cause serious irritation in your esophagus. - Avoid alcohol: While not all antibiotics react badly with alcohol, some (like metronidazole and tinidazole) can cause dangerous reactions like rapid heartbeat, vomiting, or flushing. When in doubt, skip it.Combat Antibiotic Diarrhea Before It Starts
Diarrhea is the most common reason people quit antibiotics early. But you don’t have to just endure it. Probiotics can help. Clinical trials show that taking a probiotic with Lactobacillus rhamnosus GG or Saccharomyces boulardii reduces antibiotic-associated diarrhea by about half. Look for supplements with at least 5 billion CFUs and take them 2 hours after your antibiotic dose. You can also get probiotics from plain, unsweetened yogurt. Avoid flavored yogurts-they’re full of sugar, which feeds bad bacteria. If you’re already experiencing diarrhea, stay hydrated. Drink water, broth, or oral rehydration solutions. Avoid sugary drinks and caffeine-they make diarrhea worse. If it lasts more than 48 hours after you finish your antibiotics, or if you see blood or mucus, call your doctor. That could be C. diff.Watch Out for Sun Sensitivity
If you’re taking doxycycline, tetracycline, or ciprofloxacin, your skin becomes more sensitive to sunlight. You can get sunburned in minutes-even on cloudy days. This isn’t just uncomfortable; it increases your risk of long-term skin damage. Use a broad-spectrum sunscreen with SPF 30 or higher that protects against both UVA and UVB rays. Reapply every 2 hours if you’re outside. Wear a wide-brimmed hat, long sleeves, and sunglasses. Avoid tanning beds entirely while on these antibiotics.
Recognize the Red Flags
Most side effects are annoying but harmless. But some need emergency care:- Difficulty breathing, swelling of the face or throat, or hives → possible allergic reaction
- Bloody or watery diarrhea with fever → possible C. diff infection
- Severe muscle or joint pain, tendon pain (especially with fluoroquinolones like ciprofloxacin)
- Unusual bruising, bleeding, or fatigue → possible blood cell changes
- Dark urine, yellowing skin or eyes → possible liver stress
Why Finishing the Full Course Matters
It’s a myth that you can stop antibiotics once you feel better. That’s exactly how resistant bacteria survive. When you stop early, the strongest bacteria-the ones that survived the first few doses-multiply and spread. Studies show that incomplete courses contribute to 12% of antibiotic resistance cases in the U.S. Completing your full course doesn’t mean you have to suffer. It means you’re protecting yourself and others. Antibiotic resistance is one of the top 10 global health threats, according to the World Health Organization. Every time you finish your prescription, you help keep antibiotics working for everyone.What Your Doctor Should Tell You
You shouldn’t have to figure this out alone. Good doctors don’t just hand you a prescription-they explain what to expect. According to Healthgrades, 68% of patients who finished their antibiotics said the most helpful thing was their doctor telling them, “This might happen, and here’s how to handle it.” Ask your doctor or pharmacist:- What side effects should I expect?
- Should I take this with food or on an empty stomach?
- Is there a probiotic you recommend?
- What symptoms mean I need to call you right away?

When to Call Your Pharmacist
Your pharmacist is your best ally for managing side effects. They know how your specific antibiotic interacts with food, other meds, and your health history. Many pharmacies now offer free 10-minute counseling sessions when you pick up antibiotics. Pharmacists can also help you find:- Generic alternatives with fewer side effects
- Over-the-counter remedies for nausea or diarrhea
- Probiotic brands that are clinically proven
What’s New in Antibiotic Care
In 2023, the FDA approved the first probiotic strain-Lactobacillus reuteri NCIMB 30242-specifically for preventing antibiotic-associated diarrhea. The CDC also launched a free digital tool called the “Antibiotic Side Effect Navigator” that gives personalized tips based on your antibiotic, age, and health conditions. Research is moving fast. A 2023 study found that testing your gut microbiome before prescribing antibiotics reduced side effects by 37%. In the next few years, AI tools will help doctors pick the right antibiotic for your body, not just your infection. This could cut side effects by nearly half.You Can Do This
Antibiotics are powerful, but they’re not meant to be endured blindly. You don’t need to suffer through nausea, diarrhea, or sunburn just to finish your course. With the right knowledge, you can manage side effects, stay on track, and protect your health-and the health of others. Start by asking your doctor or pharmacist: “What should I expect, and how do I handle it?” Then, follow the simple steps: take your medicine correctly, use probiotics, watch for warning signs, and finish the full course. It’s not just about feeling better now-it’s about making sure antibiotics still work when you really need them.Can I stop taking antibiotics if I feel better?
No. Feeling better doesn’t mean all the bacteria are gone. Stopping early lets the strongest bacteria survive and multiply, which can lead to a worse infection later and contributes to antibiotic resistance. Always finish your full course unless your doctor tells you to stop.
Do probiotics really help with antibiotic side effects?
Yes. Clinical trials show that probiotics like Lactobacillus rhamnosus GG and Saccharomyces boulardii reduce antibiotic-associated diarrhea by about 50%. Take them 2 hours after your antibiotic dose. Plain, unsweetened yogurt is a good food source too.
Is it safe to drink alcohol while on antibiotics?
It depends on the antibiotic. With most, moderate alcohol won’t reduce effectiveness, but it can worsen side effects like nausea or dizziness. With metronidazole or tinidazole, alcohol can cause dangerous reactions like rapid heartbeat, vomiting, or flushing. When in doubt, avoid alcohol entirely.
What should I do if I get diarrhea while on antibiotics?
Mild diarrhea is common and usually resolves on its own. Drink plenty of fluids and take a probiotic. Avoid sugary drinks and caffeine. If the diarrhea is bloody, watery, lasts more than 48 hours after finishing the antibiotic, or is accompanied by fever or severe pain, contact your doctor immediately-it could be C. diff.
Why do some antibiotics need to be taken on an empty stomach?
Antibiotics like tetracycline and doxycycline bind to calcium, iron, and dairy products, which blocks their absorption. Taking them with food or supplements can make them less effective. Always follow your doctor’s instructions on timing-some need to be taken 1 hour before or 2 hours after eating.
Can antibiotics cause long-term gut damage?
Most people’s gut bacteria recover within weeks after finishing antibiotics. But in rare cases, especially after multiple courses or prolonged use, the balance may take longer to restore. Using probiotics during and after treatment helps. If you have ongoing digestive issues, talk to your doctor about testing or specialized care.
Are there antibiotics with fewer side effects?
Yes. Some antibiotics are better tolerated than others. For example, amoxicillin is generally gentler on the stomach than clindamycin or ciprofloxacin. Your doctor can choose an alternative based on your infection, history of side effects, and other medications you take.
What should I do if I miss a dose?
If you miss a dose by a few hours, take it as soon as you remember. If it’s almost time for your next dose, skip the missed one and go back to your regular schedule. Don’t double up unless your doctor says to. Missing one dose won’t ruin your treatment, but skipping doses increases resistance risk.

Robert Bowser
October 29, 2025 AT 15:54Been on antibiotics twice this year and honestly, the probiotic tip saved me. I started taking L. rhamnosus GG right away and barely had any stomach issues. Didn't even think about quitting. Just took it with a little yogurt after my dose and kept going. Feels good knowing I didn't contribute to resistance.
Also, the part about doxycycline and sunlight? Lifesaver. Got burned bad on my first round because I didn't know. Now I wear a hat indoors near windows. Weird, but worth it.
Sue M
October 31, 2025 AT 05:26There is a critical error in the article: it states that '1 in 5 people on antibiotics experience side effects,' yet later claims 'about 25% develop diarrhea.' These figures are inconsistent and undermine credibility. Additionally, the phrase 'you don't have to suffer through them alone' is grammatically flawed-it should be 'you don't have to suffer through them alone.'
Also, the CDC’s 'Antibiotic Side Effect Navigator' is not an official tool as of 2024. Misinformation like this, even if well-intentioned, can erode public trust in medical guidance.
Tiffanie Doyle
November 1, 2025 AT 09:37OMG YES to the probiotic thing!! I was ready to quit my amoxicillin last time because my gut felt like a tornado... then my pharmacist said 'try this yogurt' and I was like okay fine 🤷♀️
Turns out plain yogurt + 2 hours after pill = magic. I finished my whole course and didn’t even feel like a zombie. Also, DO NOT drink alcohol with metronidazole. I learned that the hard way. Like, hospital hard way. Don’t be me 😅
Also, ask your doc for the side effect sheet. It’s literally free and they’ll think you’re a superhero for being prepared.
james landon
November 1, 2025 AT 14:16Bro I just take my antibiotics with a beer and call it a day. What’s the worst that could happen? I feel fine, so why stress? Also, I always stop when I feel better-why punish myself? I’ve been doing this for 10 years and I’m still standing. Maybe I’m just lucky.
Also, probiotics? Nah, I just eat yogurt. That’s basically the same thing right? 😎
Jenn Clark
November 3, 2025 AT 04:16I appreciate how practical this is. My mom was on antibiotics last winter and didn’t know about the sun sensitivity-she got a second-degree burn just walking to the mailbox. After that, we printed out the whole guide and kept it on the fridge. Now she asks her pharmacist every time.
It’s small things like this that make a huge difference. Not everyone has a doctor who explains it all. So thank you for making this clear.
L Walker
November 3, 2025 AT 21:51Interesting piece, though I’d caution against overgeneralizing. The advice on doxycycline and food varies by indication-acne vs. Lyme disease-and the guidelines aren’t universal. Also, the claim that 12% of resistance cases stem from incomplete courses is debated; some meta-analyses suggest the link is weaker in community settings.
Still, the probiotic recommendations are solid. I’ve recommended Saccharomyces boulardii to patients for years. The 2-hour gap matters. Don’t mix it into your smoothie with the pill.
And yes-pharmacists are underrated heroes. Talk to yours.
giri pranata
November 5, 2025 AT 09:24Bro in India we just take antibiotics with milk because ‘it’s easier on the stomach’-and then wonder why we get resistant infections. This article is a wake-up call.
My cousin finished his full course after learning about C. diff from a YouTube video (yes, really). Now he’s the family antibiotic guru. We all ask him before we start anything.
Also, probiotics are not optional. They’re like a shield. Take them. Plain yogurt. No sugar. No flavor. Just pure culture. Your gut will thank you 🙏
Stuart Rolland
November 6, 2025 AT 08:39I’ve been on antibiotics so many times I’ve lost count-some for pneumonia, some for sinus infections, once even for a weird skin rash that turned out to be a fungus but they gave me amoxicillin anyway because ‘it can’t hurt.’
And you know what? I’ve always finished every single course. Not because I’m some kind of saint, but because I’ve seen what happens when you don’t. My uncle got C. diff after skipping his last few pills-he was in the hospital for three weeks, lost 30 pounds, and now he can’t eat dairy without panicking.
And yeah, the probiotics? I started taking them after my last round and honestly? I didn’t even notice the diarrhea. I just felt… normal. Like I could eat breakfast without feeling like I was going to die.
Also, the sunlight thing? I got sunburned on my chest while taking cipro last summer and it looked like I’d been whipped with a rope. I didn’t even realize it was the antibiotic until my pharmacist yelled at me. Now I wear SPF 50 even when I’m just walking the dog.
And don’t get me started on the ‘I feel better’ myth. You’re not a superhero. The bacteria are. They’re the ones that survive. And they don’t care how you feel. They just want to multiply.
So yeah. Take the pill. Take the probiotic. Drink the water. Wear the hat. Ask the pharmacist. Finish the course. It’s not hard. It’s just… necessary. And honestly? It’s the least you can do for the next person who needs antibiotics. Because if we all keep doing this, maybe one day they’ll still work.
And if you’re reading this and you’re about to quit? Just… don’t. Just one more day. Just one more pill. You’ve got this.