Why Medication Storage in Shared Homes Is a Silent Crisis
Imagine this: your teenager grabs a bottle from the bathroom cabinet thinking it’s cough syrup. It’s actually your father’s blood pressure pill. Or your roommate leaves their insulin on the fridge door, where the temperature swings 10 degrees every time someone opens it. These aren’t hypotheticals-they happen every day in shared living spaces, from multi-generational homes to group residences. And the consequences? Hospital visits, lost medication effectiveness, even death.
According to a 2025 survey by SeniorHelpers, 67% of families living with seniors reported at least one medication-related incident in the past year. Nearly half of those involved children or other residents accidentally taking pills. Meanwhile, in assisted living facilities, 22% of homes couldn’t prove they were keeping medications at the right temperature. That’s not just negligence-it’s a systemic risk.
The problem isn’t that people are careless. It’s that no one ever taught them how to do this right. Medications aren’t like cereal or shampoo. They need specific conditions to stay safe and effective. And when multiple people with different needs share a space, the risk multiplies.
What You Need to Know About Medication Storage Rules
There’s no federal law saying you must lock up your pills at home-but there should be. In professional settings like assisted living, it’s mandatory. The Joint Commission, which sets healthcare standards across the U.S., requires all medications to be stored under lock and key. And they mean it: between 2020 and 2021, 13% of hospitals got cited for failing to follow this rule.
Even in homes, state laws are catching up. As of 2025, 47 U.S. states have specific rules for medication storage in assisted living. While those don’t directly apply to private households, they set the standard. The same principles-security, temperature control, labeling, and documentation-should guide everyone.
Here’s what the experts say you must do:
- Lock it up. Any pill that isn’t in active use should be in a locked container. Not a drawer. Not a cabinet with a child lock. A real lock.
- Keep it cool. Insulin, eye drops, liquid antibiotics, and some psychiatric meds need refrigeration. But not just anywhere in the fridge. The center shelf, away from the door, is the only safe spot. Temperature swings above 46°F or below 36°F can destroy potency.
- Label everything. If a pill bottle doesn’t have the person’s name, dosage, and expiration date clearly printed, it’s a hazard. Pharmacy blister packs help-but if you’re using original bottles, write on them with a permanent marker.
- Throw out the old stuff. Expired meds are dangerous. A 2023 FDA update found that 10% of facilities had expired medications still in circulation. That includes antibiotics that lose effectiveness after expiration, turning into breeding grounds for resistant bacteria.
Setting Up a Safe Storage System at Home
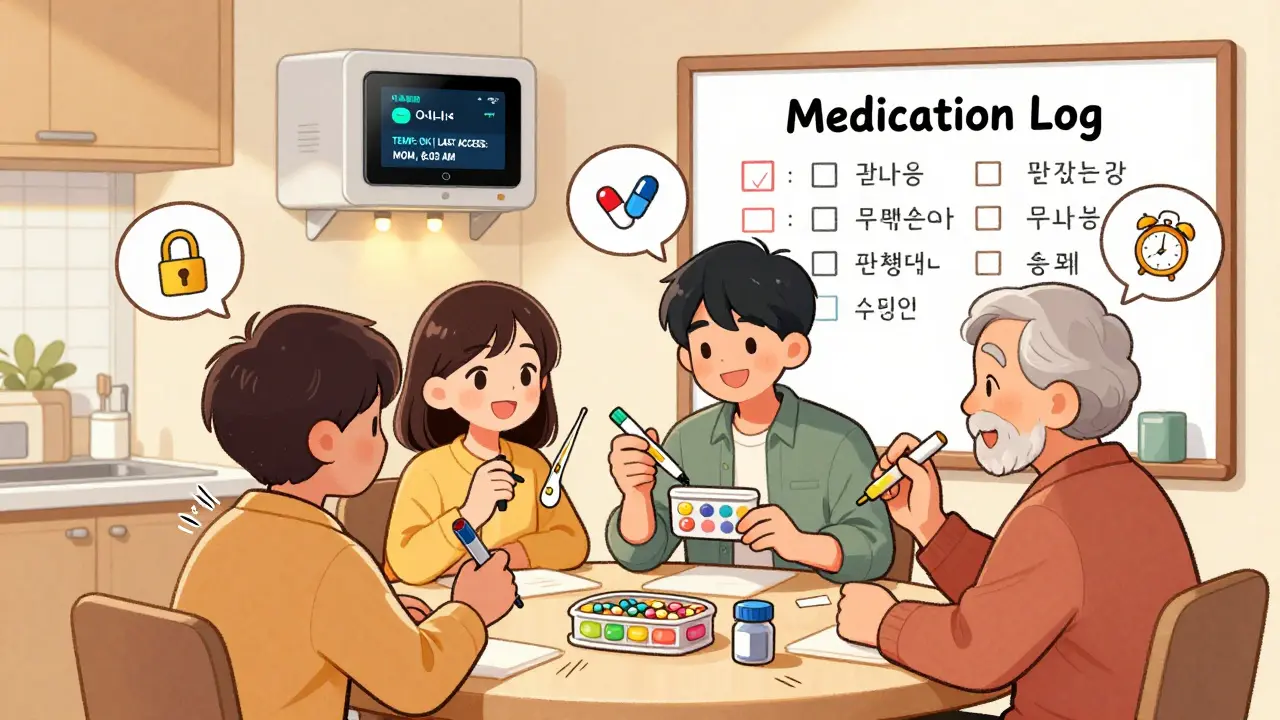
If you live with family, roommates, or aging parents, you don’t need a medical facility to keep meds safe. You just need a plan. Here’s how to build one in three steps:
- Clean house first. Gather every pill, patch, liquid, and inhaler in the house. Check expiration dates. Discard anything old, discolored, or unlabeled. Use a drug take-back program or mix pills with coffee grounds and cat litter before tossing them in the trash. Never flush them.
- Categorize by need. Group meds into three piles: daily use (like blood pressure or insulin), as-needed (painkillers, anxiety meds), and emergency (EpiPens, naloxone). Store each group differently.
- Designate zones. Create one locked storage spot for all meds. A small, portable safe with a key or code works best. Keep it in a bedroom, not the kitchen or bathroom. Bathrooms are humid, hot, and accessible to kids. Bedrooms are private, stable, and controllable.
For daily meds, use a pill organizer with compartments for morning, afternoon, evening, and night. Fill it weekly. For insulin or other refrigerated meds, use a separate, labeled container in the fridge’s center shelf. Tape a note to the fridge: “Medications Only. Do Not Touch.”

Temperature Is Everything-Here’s How to Get It Right
Medications aren’t like wine. They don’t age well on the counter. Heat, moisture, and temperature swings break them down. A 2024 Johns Hopkins study found that some antibiotics lose up to 30% of their potency within 24 hours if stored above room temperature.
Here’s what you need to know about common meds and their storage needs:
- Insulin - Must stay between 36-46°F. Never freeze. Once opened, it lasts 28 days at room temp-but only if kept under 77°F. Store in the fridge until ready to use.
- Liquid antibiotics - Many need refrigeration. Check the label. If it says “keep refrigerated,” don’t ignore it.
- Eye drops - Some require refrigeration after opening. Others don’t. Read the instructions. A 2023 Eper.com case study showed a patient’s glaucoma meds became ineffective after being left on the bathroom counter for two weeks.
- Epinephrine (EpiPen) - Keep at room temperature (68-77°F). Don’t refrigerate or leave in a hot car. If it turns cloudy or brown, throw it out.
- Controlled substances - Opioids, benzodiazepines, stimulants-these need the tightest control. Lock them in a separate compartment. Use a digital safe that logs access. If someone else takes them, even once, it’s a crime and a health emergency.
Buy a small fridge thermometer and keep it next to your meds. Check it weekly. If it goes out of range, move the meds immediately. A $10 thermometer could save a life.
Security: Locks, Keys, and Access Control
Locks aren’t just for thieves. They’re for kids, confused seniors, and well-meaning but unaware roommates. In a 2025 survey, 63% of families said they resisted locking up meds because “it’s too much work” or “we trust each other.” That trust gets broken every day.
Here’s how to handle access:
- One lock, one key. Give the key to one responsible person-usually the main caregiver. No one else gets a copy.
- Use digital safes. Smart medication safes (like those from DosePacker) cost $80-$150 and record who opens them and when. They’re worth it if you’re managing controlled substances or have a history of misuse in the household.
- Never leave meds on nightstands. Even “just for tonight.” That’s how accidents happen.
- Teach kids early. Tell them: “These aren’t candy. If you touch them without permission, someone could get very sick.”
For shared spaces with multiple residents, assign one person to manage the stash. Rotate the role monthly. Keep a simple log: “Date, Med Name, Dose Taken, Who Administered.” It takes two minutes a day. But if something goes wrong, that log could prove you did everything right.
What Works in Assisted Living vs. Your Home
Assisted living facilities use systems you can adapt:
- Blister packs. Medications are pre-sorted by day and time in plastic bubbles. No confusion. No miscounts. You can get these from your pharmacy for a small fee.
- Dedicated medication rooms. Large facilities have locked rooms with refrigerators just for meds. You can’t do that at home-but you can mimic it. Use a locked box on a shelf in a quiet room.
- Electronic records. Staff log every dose given. You can use a simple app like Medisafe or MyTherapy to track doses, set reminders, and alert you if one’s missed.
The biggest difference? Professional settings have training. Staff get 8-12 hours of initial instruction. Families get Google. Start your own training: watch a 10-minute video from the FDA on proper storage. Read the label on every bottle. Ask your pharmacist: “What’s the one thing I should never do with this?”
What’s Changing in 2025 and Beyond
The world of medication storage is getting smarter. In 2024, DosePacker launched smart cabinets that monitor temperature and humidity, send alerts if something’s wrong, and log every access. By 2027, 65% of care facilities will use them.
For homes, the market is catching up. Sales of home medication safes jumped 27% in 2024. Companies like SeniorHelpers now offer certification programs for family caregivers-12,500 people signed up in the first month of 2025.
And AI is coming. Beta systems are testing computer vision to spot if a pill bottle was left open or if a fridge door stayed ajar too long. These aren’t sci-fi. They’re the next step.
But you don’t need AI to stay safe. You just need awareness, a lock, and a little discipline.
What to Do If Something Goes Wrong
Even with the best system, mistakes happen. Here’s what to do:
- Someone took a pill by accident? Call Poison Control immediately (1-800-222-1222 in the U.S. and Canada). Don’t wait for symptoms. Have the pill bottle ready.
- Medication was left out overnight? Check the label. If it says “store in refrigerator,” and it was warm for more than 24 hours, throw it out. Better safe than sorry.
- You’re not sure if a pill is expired? When in doubt, toss it. Pharmacies will take back old meds for free. Use their drop boxes.
- Someone’s misusing meds? Talk to a doctor or counselor. This isn’t a discipline issue-it’s a medical one. Get help before it escalates.
Don’t hide mistakes. Report them. The sooner you fix the system, the safer everyone becomes.


Corey Chrisinger
January 17, 2026 AT 06:12Ryan Hutchison
January 18, 2026 AT 14:09evelyn wellding
January 19, 2026 AT 09:16Chelsea Harton
January 19, 2026 AT 19:29brooke wright
January 19, 2026 AT 21:22Nick Cole
January 21, 2026 AT 01:57waneta rozwan
January 21, 2026 AT 14:25john Mccoskey
January 23, 2026 AT 05:41Samyak Shertok
January 24, 2026 AT 02:00Joie Cregin
January 25, 2026 AT 23:32Melodie Lesesne
January 26, 2026 AT 05:41Rob Deneke
January 27, 2026 AT 22:00Bianca Leonhardt
January 29, 2026 AT 18:18Travis Craw
January 31, 2026 AT 14:00