Every year, millions of people in the U.S. get the wrong medication, the wrong dose, or wrong instructions - not because of malice, but because of system flaws. Medication errors are one of the most common - and preventable - causes of harm in healthcare. But here’s the twist: the kind of mistake you’re likely to face in a hospital isn’t the same as the one you might get at your local pharmacy. And knowing the difference could save your life.
How Often Do Errors Happen?
In hospitals, errors are everywhere. A 2006 study across 36 hospitals and nursing homes found that nearly 1 in every 5 doses contained some kind of mistake. That’s 20%. Nurses give the wrong drug. The wrong time. The wrong amount. It happens during prescribing, transcribing, dispensing, and especially during administration. In fact, the most common point of failure is when the nurse hands you the pill - not when the pharmacist fills the bottle. Now compare that to your neighborhood pharmacy. Retail pharmacies fill about 3 billion prescriptions each year. Studies estimate that around 1.5% of those prescriptions have an error. That sounds low - until you do the math. 1.5% of 3 billion is 45 million mistakes annually. That’s not a few bad apples. That’s a system-wide issue. Here’s the real difference: hospitals have layers of checks. Nurses verify what the pharmacist gave. Pharmacists double-check orders. Electronic alerts flag dosage issues. In retail pharmacies? You’re often the last line of defense. The pharmacist fills the script. You walk out. No one checks if you got the right thing. And if you don’t know what you’re supposed to be taking? You might never realize it’s wrong.What Kind of Mistakes Happen Where?
In community pharmacies, the top three errors are simple but deadly:- Wrong medication (giving lisinopril instead of losartan)
- Wrong dose (10 mg instead of 1 mg)
- Wrong instructions (‘take twice a day’ instead of ‘take twice a week’)
Why Do These Errors Happen?
In retail pharmacies, the biggest culprit isn’t laziness - it’s pressure. Pharmacists are expected to fill 250 prescriptions a day. That’s about 1 every 2 minutes. And most errors come from cognitive overload. The pharmacist is distracted. The system auto-fills a wrong dose. The label printer glitches. The pharmacy is understaffed. A 2023 AHRQ report found that 80% of community pharmacy errors are tied to how the workplace is organized - not the individual pharmacist’s skill. In hospitals, the problem is communication. Doctors write unclear orders. Nurses miss handoffs between shifts. Electronic systems don’t talk to each other. A patient gets transferred from ICU to a regular floor, and the new team doesn’t realize the insulin dose was cut in half. Staff are overworked. Burnout is high. And unlike pharmacies, hospitals don’t always track near-misses - only actual harm.
Who Gets Hurt the Most?
In retail pharmacies, patients are often older, taking multiple medications, and managing chronic conditions like diabetes, heart disease, or blood clots. A mistake with warfarin, insulin, or digoxin can send someone to the ER - or worse. The NIH found that 1 in every 10,000 community pharmacy errors led to hospitalization. That’s rare per script, but with 45 million errors a year, that’s still thousands of hospitalizations. In hospitals, patients are sicker. They’re on IV drips, ventilators, and multiple high-risk drugs. An error here can kill faster. A 2022 study showed that 7,000 to 9,000 deaths each year in the U.S. are tied to medication errors - most of them happening in hospitals. But here’s the catch: hospitals catch more errors before they hurt patients. A nurse notices the wrong drug and stops it. A pharmacist calls the doctor to clarify. In retail pharmacies, that safety net doesn’t exist.How Are Errors Reported?
Hospitals have formal reporting systems. If a nurse gives the wrong dose, they fill out a form. It goes to a safety team. They analyze it. They change procedures. Some large hospitals report over 100 medication errors per month - and that’s just the ones they catch. Community pharmacies? Not so much. Until recently, most didn’t report errors at all. The FDA gets over 100,000 reports a year - but experts say that’s less than 1% of what actually happens. California now requires pharmacies to log all errors and show them during inspections. Other states are following. But most still rely on patients to speak up - and most patients don’t know what to look for.
What’s Being Done to Fix This?
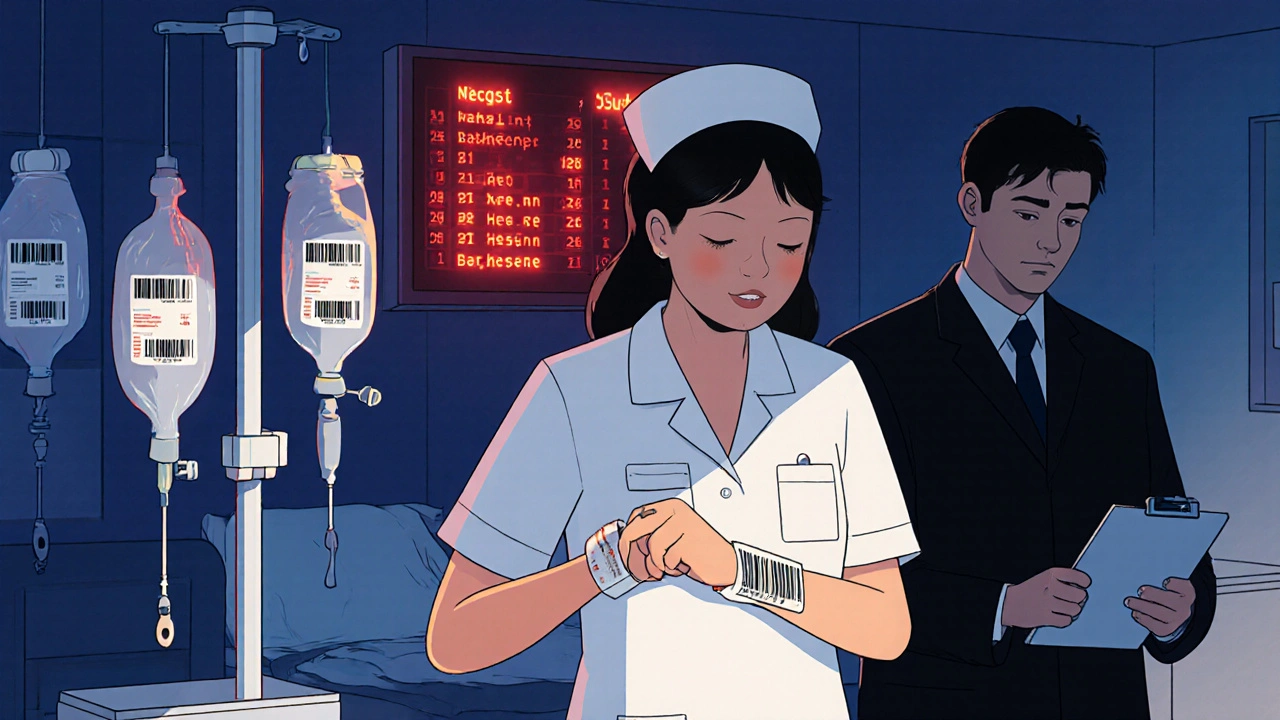
Hospitals are using barcode scanning. Nurses scan the patient’s wristband and the drug’s barcode before giving anything. This cuts errors by up to 86%. Electronic health records now flag dangerous drug interactions. Automated dispensing machines reduce human input. Retail pharmacies are catching up. CVS Health rolled out AI-powered verification in 2022. It scans prescriptions for dosage red flags and catches 37% more errors before they leave the counter. Mayo Clinic’s integrated system reduced hospital errors by 52%. The CDC and FDA are pushing for standardized reporting across all pharmacy settings. By 2024, new AI tools are being tested to catch transcription errors - the most common cause of community pharmacy mistakes - with early results showing up to 63% fewer errors in pilot programs.What Can You Do?
You’re not powerless. Here’s what works:- Always ask: ‘What is this medicine for?’ and ‘How should I take it?’
- Check the label against the prescription slip your doctor gave you.
- If the pill looks different than last time - ask why.
- Keep a list of all your meds - including doses and times - and bring it to every appointment.
- If you’re in the hospital, don’t assume the nurse knows your meds. Say: ‘I take 5 mg of metoprolol every morning. Is that what you’re giving me?’
The Bottom Line
Hospitals have more errors - but more safeguards. Retail pharmacies have fewer errors - but fewer checks. The real danger isn’t the number. It’s the silence. In hospitals, mistakes are tracked and fixed. In pharmacies, they often go unnoticed - until someone gets hurt. The system isn’t broken. It’s unbalanced. Fixing it means better tech in pharmacies, better training for staff, and - most importantly - patients who know their rights and aren’t afraid to ask questions.What’s the most common type of medication error in retail pharmacies?
The most common error is incorrect instructions - like telling a patient to take a pill twice a day when the doctor meant twice a week. Other frequent errors include giving the wrong medication or the wrong dose. These often happen because pharmacists are rushed, automated systems misread handwriting, or labels are printed incorrectly.
Are hospital medication errors more dangerous than pharmacy errors?
It depends. Hospital errors happen more often and involve sicker patients, so when they cause harm, the results can be immediate and severe - like cardiac arrest from an incorrect IV dose. But pharmacy errors are more likely to go unnoticed for days or weeks, leading to long-term damage like kidney failure from chronic overdosing. Both are dangerous; the difference is speed versus stealth.
Why don’t pharmacies report more errors?
Many pharmacies fear legal consequences or loss of reputation. Until recently, there was no national requirement to report. Even now, only a few states like California enforce reporting. Most errors are never documented unless they cause obvious harm. This makes it hard to track trends or fix root causes.
Can technology reduce medication errors?
Yes - and it already is. Barcode scanning in hospitals has cut administration errors by 86%. AI tools in pharmacies now flag incorrect doses and drug interactions before a prescription is filled. CVS and other chains report 30-60% fewer errors after implementing these systems. But tech alone isn’t enough. Staff training and a culture that encourages reporting are just as important.
What should I do if I think I got the wrong medication?
Don’t wait. Call your pharmacist immediately and ask to speak to the pharmacist on duty. Bring the bottle and your prescription slip. If you’re already taking it and feel unusual symptoms - dizziness, nausea, rapid heartbeat - stop taking it and call your doctor or go to urgent care. Never assume it’s a mistake you imagined. Trust your instincts.
Are generic drugs more likely to cause errors?
No. Generic drugs are just as safe and effective as brand names. But they can cause confusion if the name looks similar to another drug - like ‘Lisinopril’ vs. ‘Losartan.’ Pharmacists are trained to spot these, but mistakes still happen. Always check the active ingredient on the label, not just the brand or generic name.

Andrew McAfee
November 24, 2025 AT 22:25So hospitals are full of mistakes but at least they catch em
Pharmacies? You get your pills and hope for the best
My grandma took blood thinner wrong for 3 months cause the label said daily instead of weekly
She almost died
And no one ever apologized
Srikanth BH
November 25, 2025 AT 08:58This is so true and I’m glad someone finally put it this clearly
People think pharmacists are just order-takers but they’re under insane pressure
I’ve seen my uncle work 12-hour shifts with 200 scripts to fill
One wrong label and someone’s life changes forever
We need better systems not just blame
Ellen Sales
November 26, 2025 AT 11:34Okay, I’ve been a nurse for 22 years and let me tell you - the hospital system is a mess, but at least we have barcode scanners and double-checks
At my last job, we caught 17 errors in one shift just because someone paused to verify
But the pharmacy? No one’s checking your meds after you walk out
And don’t get me started on how often they give you the wrong pill because the bottle looked similar
It’s not incompetence - it’s design failure
And yes, I’ve seen patients die because no one asked if the blue pill was supposed to be white
And no one ever asks because they think the system works
It doesn’t
And we’re all paying for it
And if you think your pharmacist is ‘just busy’ - imagine being the one who got the wrong dose of insulin
And no one ever says sorry
It’s not a glitch
It’s a crisis
giselle kate
November 27, 2025 AT 22:28Of course hospitals have more errors - they’re run by unionized bureaucrats who think ‘process’ is a cure
Meanwhile, pharmacies are run by actual professionals who’ve been doing this for decades
But no, let’s blame the pharmacist because the system’s broken
Wake up - the real problem is the government and insurance companies squeezing everyone dry
Stop blaming the workers
They’re doing their best with broken tools
And if you think AI is gonna fix this - you’ve never worked in a pharmacy
It’s not tech - it’s respect
And we don’t have any left
Emily Craig
November 28, 2025 AT 08:41Y’all are acting like this is news
My mom got the wrong blood pressure med and ended up in the ER
She didn’t even know until she saw the pill color was different
And the pharmacist said ‘oh yeah we ran out of the other one’
Like that’s a thing you say to someone who’s been taking it for 10 years
So now I carry a laminated card with every med I take
And I ask EVERY TIME
And I don’t care if I sound annoying
Because I’d rather be annoying than dead
And if you’re not doing this - you’re playing Russian roulette with your health
And no one’s coming to save you
Not the system
Not the pharmacist
Just you
So do it
Now
Karen Willie
November 28, 2025 AT 17:43I’ve worked in community health for 15 years and I can tell you - the quietest victims are the elderly
They don’t speak up because they don’t want to be a burden
Or they don’t understand the meds
Or they’re scared to challenge the ‘expert’
But if you visit an older patient’s home - look at their pill organizer
Chances are, it’s a mess
And no one’s checking
We need more home visits
More pharmacist outreach
More time
Not just tech
Because tech doesn’t care if someone’s lonely
And loneliness makes mistakes worse
Andrew Camacho
November 28, 2025 AT 22:44Oh wow - hospitals are bad, pharmacies are worse - shocker
Let me guess, next you’ll tell me the sun rises in the east
And that the FDA is useless
And that pharmacists are overworked
Newsflash - EVERYTHING is broken
But you want to fix it by making patients into medical detectives?
That’s not a solution - that’s surrender
And the real problem? We’ve outsourced responsibility to the consumer
When did it become YOUR job to catch the system’s mistakes?
It shouldn’t be
It’s not your fault
It’s the system’s
And until we stop blaming the patient and start holding institutions accountable - nothing changes
And yes, I’m mad
And you should be too
Arup Kuri
November 30, 2025 AT 01:59They don’t want you to know this but the whole thing is rigged
Big Pharma pays the pharmacists to push certain meds
And the hospitals? They get paid more if you stay longer
So they keep giving you drugs even when you don’t need them
And the AI? It’s just a cover-up
They use it to look like they’re fixing things while they keep the same broken model
You think the government cares?
They get their kickbacks
And you? You’re just a number
Wake up
They’re not trying to help you
They’re trying to profit off your pain
Elise Lakey
December 1, 2025 AT 22:00I’m curious - how many of these errors are caught by patients who actually read the labels?
Because I’ve had pharmacists say ‘it’s the same thing’ when the dose changed
And I asked - and they admitted they didn’t check the script
So I started writing down the drug name, dose, and purpose on my phone before I leave the counter
It’s not hard
But I’ve never met anyone else who does it
Is it just me?
Or are people just trusting too much?
Roscoe Howard
December 2, 2025 AT 06:18It is imperative to underscore the fact that the current paradigm of pharmaceutical dispensation is predicated upon a structural deficit in human capital allocation and institutional oversight
Furthermore, the confluence of fiscal austerity measures and regulatory fragmentation has engendered a pernicious environment wherein pharmacists are compelled to operate under conditions antithetical to patient safety
One must consider the empirical data presented by the AHRQ - 80% of errors are attributable to systemic design flaws rather than individual negligence
Therefore, it is not merely advisable - it is ethically obligatory - to advocate for comprehensive policy reform
And until such time as the federal government mandates standardized reporting protocols across all pharmacy settings - we are merely rearranging deck chairs on the Titanic
Kimberley Chronicle
December 3, 2025 AT 05:49Interesting analysis - the differential in error profiles between acute care and ambulatory settings is well-documented in the literature
But what’s underreported is the cognitive load differential - pharmacists in retail face higher task-switching frequency and lower decision-support integration
That’s why AI-driven verification tools are so critical - they reduce the bandwidth required for error detection
And the fact that CVS saw a 37% reduction? That’s not just tech - that’s systems engineering working as intended
Still - the human factor remains non-negotiable
Technology augments - it doesn’t replace
And we need both
Shirou Spade
December 4, 2025 AT 14:26It’s funny how we treat medicine like it’s a science when it’s really a ritual
We give people pills like they’re magic beans
And then act shocked when things go wrong
But the real question isn’t who’s making the mistake
It’s why we think a pill can fix everything
Maybe we need less drugs
And more listening
More time
More care
Not just better labels
Lisa Odence
December 6, 2025 AT 01:28OMG this is so important 😭 I’ve been telling everyone about this for years!
My cousin got the wrong chemo med and it almost killed her 💔
And the pharmacy said ‘oops’ and gave her a coupon for 10% off 😒
That’s not enough
We need REAL accountability
And AI should be mandatory in every pharmacy
Like, right now
And if you’re not checking your meds - you’re basically signing a waiver to die
So please
Just ask
Just check
Just care
❤️❤️❤️