Bladder Pain Relief Estimator
How Physical Therapy Can Help Your Pain
Based on clinical studies, physical therapy for bladder pain can reduce pain levels by 30-50% within 6 weeks. This calculator estimates your potential improvement based on your current pain level.
Imagine a day without the constant urge to run to the bathroom or the sharp, cramping pain that makes you tense up every time you sit. For many people dealing with bladder pain, that day feels impossible-until they discover physical therapy for bladder pain. This approach doesn’t rely on pills or invasive procedures; instead, it trains the muscles and nerves that control the bladder, easing discomfort and restoring confidence.
What Physical Therapy Does for Bladder Pain
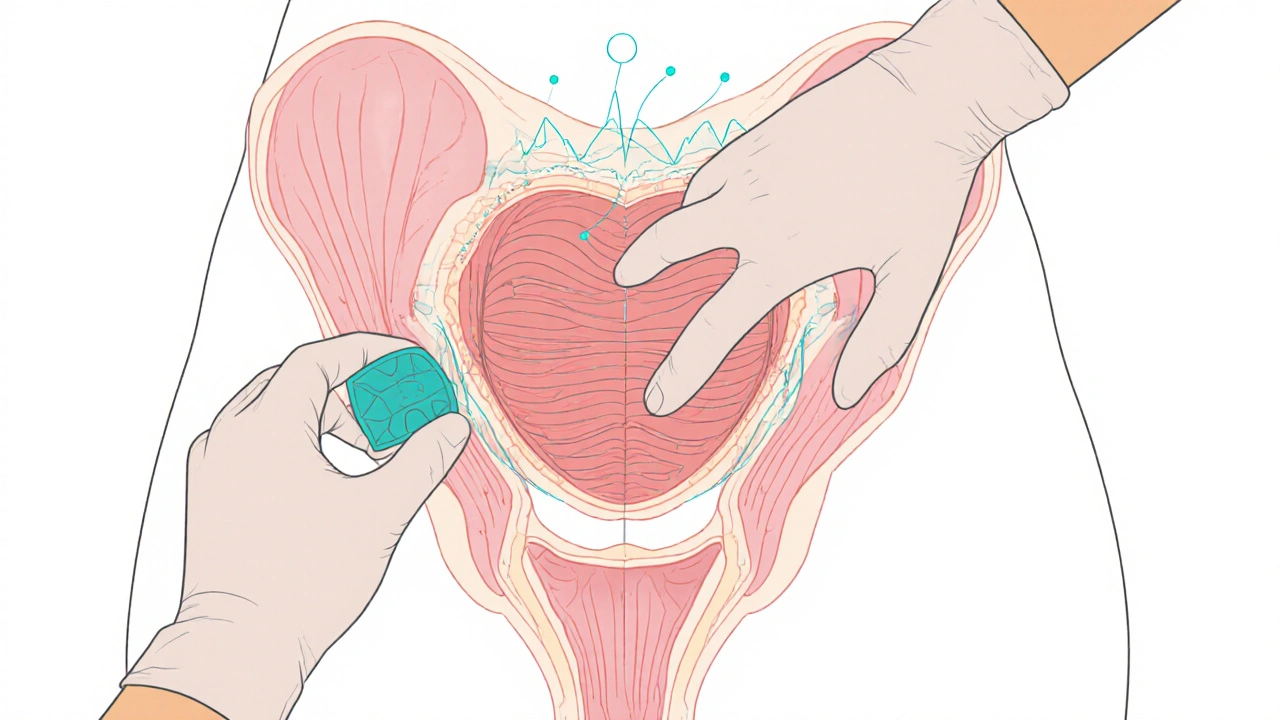
When you hear Physical therapy, you might picture a therapist helping you recover from a broken leg. In the context of bladder pain, the focus shifts to the Pelvic floor. This muscular sling supports the bladder, urethra, and surrounding organs. If the muscles become tight, weak, or hyper‑active, they can trigger pain, urgency, and incomplete emptying.
Therapists use a blend of manual techniques, biofeedback, and exercise prescription to relax over‑active fibers, improve strength where it’s lacking, and re‑educate the nervous system. The result is a calmer bladder, less pain, and fewer trips to the restroom.
Core Techniques Used in Bladder‑Focused PT
- Myofascial release: Hands‑on pressure that loosens the fascia surrounding the pelvic muscles, reducing trigger points that can refer pain to the bladder.
- Biofeedback: Sensors attached to the perineum give real‑time visual cues, helping patients learn to contract and relax the pelvic floor correctly.
- Trigger point therapy: Direct pressure on painful knots within the obturator internus or levator ani muscles, often the source of deep pelvic ache.
- Kegel exercises (when taught correctly): Targeted strengthening that improves bladder control, but only after the muscles are first relaxed.
- Pelvic floor motor retraining: A step‑by‑step program that alternates relaxation and activation to break the cycle of chronic tension.
Direct Benefits You’ll Notice
Clinical trials and real‑world case series consistently report four main gains:
- Pain reduction: Patients often experience a 30‑50% drop in average pain scores within six weeks.
- Improved bladder control: Urgency episodes shrink by about 40% and nighttime trips drop dramatically.
- Less reliance on medication: Many users can taper off anticholinergics or opioids after a course of PT.
- Enhanced quality of life: Surveys show higher scores on the SF‑36 mental and physical components after therapy.
Who Stands to Gain the Most
The approach shines for several diagnostic groups:
- Interstitial cystitis (painful bladder syndrome) - where the bladder lining is inflamed and muscle spasm worsens symptoms.
- Chronic pelvic pain syndrome - often linked to hypertonic pelvic muscles that mimic bladder pain.
- Post‑surgical patients - after hysterectomy or prostate surgery, the pelvic floor can become scarred and tight.
- Women with recurrent urinary tract infections - PT can break the cycle of irritation and muscle over‑activity.
What a Typical Session Looks Like
First, the therapist conducts a thorough assessment: a bladder diary review, digital pelvic exam, and sometimes surface EMG to map muscle activity. Based on the findings, a personalized plan unfolds:
- Assessment & education: You learn why the pelvic floor matters and what habits may be aggravating pain.
- Manual therapy: Myofascial release and trigger point work target tight spots.
- Biofeedback training: Visual feedback helps you gain voluntary control over relaxation.
- Home exercise program: Simple stretches, diaphragmatic breathing, and correctly performed Kegels.
- Progress review: Every 2‑3 weeks the therapist adjusts intensity and adds new tools (e.g., electrical stimulation if needed).
Most patients attend 8‑12 weekly sessions, but many notice meaningful change after just four.

Physical Therapy vs. Other Treatment Paths
| Treatment | Effectiveness (short‑term) | Invasiveness | Typical Side Effects | Average Cost (US) | Best For |
|---|---|---|---|---|---|
| Physical therapy | ~45% pain reduction | Non‑invasive | Temporary soreness | $150‑$250 per session | Muscle‑related pain, chronic cases |
| Medication (anticholinergics) | ~30% pain reduction | Oral | Dry mouth, constipation | $30‑$100 per month | Acute urgency, short‑term relief |
| Surgery (e.g., bladder augmentation) | ~60‑70% reduction | Highly invasive | Infection, recovery time | $15,000‑$30,000 | Severe refractory cases |
Physical therapy sits in the sweet spot: solid effectiveness without the risks of drugs or surgery.
Choosing the Right Therapist and Getting the Most Out of PT
- Look for a licensure in Pelvic health physical therapy or a certification from the American Physical Therapy Association’s Pelvic Health section.
- Ask about experience with interstitial cystitis or chronic pelvic pain.
- Make sure the clinic has biofeedback equipment - a reliable indicator of modern practice.
- Commit to the home program; consistency beats intensity.
- Track symptoms in a bladder diary; data helps the therapist fine‑tune treatment.
Frequently Asked Questions
Can physical therapy cure bladder pain?
It rarely "cures" the underlying disease, but it can dramatically lower pain, urgency and medication use for most patients when combined with proper medical care.
How long before I feel relief?
Many notice improvement after 4-6 sessions (about 1-2 months). Full benefit often appears after 8‑12 weeks of regular work.
Is PT painful?
Some discomfort is normal during manual release, but the therapist will adjust pressure. The goal is to ease tension, not cause injury.
Do I need a doctor’s referral?
In many states you can self‑refer to a pelvic‑health PT. However, a physician’s diagnosis helps insurance and ensures the right underlying cause is addressed.
Can men benefit from this therapy?
Absolutely. Male pelvic floor dysfunction after prostate surgery or chronic prostatitis often presents as bladder pain, and PT techniques are identical.


Catherine Zeigler
October 11, 2025 AT 23:24I’ve seen so many people stuck in the endless cycle of pain and medication, and this article really shines a light on a gentle alternative. The way you break down the pelvic floor techniques makes it feel approachable even for beginners. I love how you emphasize the importance of a skilled therapist and biofeedback, because those details can be game‑changers. It’s reassuring to hear that most patients notice improvements after just a few sessions, giving hope to those who feel hopeless. The comparison table does a great job of putting PT side‑by‑side with drugs and surgery, highlighting the non‑invasive nature. Your tips on choosing the right therapist are spot on – certification and equipment matter. I also appreciate the practical home‑exercise suggestions; consistency really does beat intensity. Keep spreading this empowering information – it can change lives. Thank you for the thorough, compassionate guide.
henry leathem
October 14, 2025 AT 06:57While the article is well‑intentioned, it glosses over the complex neurophysiology that underlies bladder pain syndromes. The reliance on vague terms like “manual therapy” without quantifiable metrics is intellectually lazy. Moreover, the claimed 30‑50% reduction lacks citation of rigorous double‑blind trials. Patients deserve evidence‑based protocols, not anecdotal optimism mixed with buzzwords.
jeff lamore
October 16, 2025 AT 11:44Thank you for the clear layout; it respects the reader’s need for both detail and brevity. The step‑by‑step session outline is particularly useful for newcomers. I would add a brief note on insurance coverage, as many are concerned about cost. Overall, it balances professionalism with accessibility nicely.
Kris cree9
October 18, 2025 AT 13:44this sounds like a miracle cure but i bet there’s a catch.
i’ll believe it when i see someone actually stop crying in the bathroom.
Paula Hines
October 20, 2025 AT 12:57The philosophical underpinnings of pelvic health are often ignored in mainstream discourse. By treating the bladder as an isolated organ we miss the systemic interconnectedness that defines the human experience. Physical therapy addresses the myofascial continuum, allowing the body to re‑establish homeostasis. It is not merely a set of exercises but a re‑education of somatic awareness. When we train the pelvic floor we are, in effect, re‑programming the autonomic nervous system. This resonates with ancient practices that sought balance rather than suppression. The article’s emphasis on biofeedback mirrors the concept of reflective consciousness, turning internal signals into actionable data. Moreover, the reduction in medication reliance aligns with the principle of non‑interventionist healing. One must also consider the sociocultural stigma attached to pelvic pain, which often prevents patients from seeking help. By providing a non‑invasive option we empower individuals to reclaim agency over their bodies. Finally, the cost‑benefit analysis presented underscores the value of preventive care in a consumer‑driven healthcare model. In sum, PT for bladder pain is a sophisticated, holistic approach that honors both the physiological and existential dimensions of suffering.
John Babko
October 22, 2025 AT 09:24Absolutely!!! This is the kind of evidence‑based, patient‑centered care we need!!! The data presented is compelling, and the practical tips are gold!!! I especially appreciate the emphasis on therapist certification!!! It shows a commitment to standards!!! Let’s spread the word and get more people into these programs!!!
Stacy McAlpine
October 24, 2025 AT 03:04Great rundown! I’ve been curious about pelvic health and this breaks it down in a way that’s easy to understand. The cultural tip about keeping a bladder diary is actually a smart habit for anyone. It’s also cool to see the inclusive note that men can benefit too. Definitely sharing this with friends who deal with chronic discomfort.
Roger Perez
October 25, 2025 AT 17:57Wow, this is super helpful! 😊 The explanation of myofascial release made a lot of sense to me. I love that the article stresses both relaxation and proper activation – balance is key! 🙏 If you’re on the fence, give PT a try – the numbers speak for themselves. 🌟
michael santoso
October 27, 2025 AT 05:04The discourse here suffers from a paucity of critical appraisal. One must interrogate the methodological rigor of the cited “clinical trials.” The absence of control groups and blinding raises questions about internal validity. Furthermore, the cost analysis neglects socioeconomic disparities that affect access. While the physiological rationale is plausible, a more nuanced synthesis is required before endorsing PT as a panacea.
M2lifestyle Prem nagar
October 28, 2025 AT 14:24Try PT for bladder pain, it works.
Karen Ballard
October 29, 2025 AT 20:57Love the detail! 🙌 Especially the part about biofeedback making the nervous system more cooperative. 👍 Keep the info coming!
Gina Lola
October 31, 2025 AT 00:44That table is fire, really shows PT’s sweet spot. The jargon is on point and the vibe feels chill. Nice work.
Leah Hawthorne
November 1, 2025 AT 01:44Thanks for the thorough guide. I especially liked the home‑exercise suggestions – they’re simple enough to fit into a busy day. The tone feels friendly and not condescending.
Brian Mavigliano
November 1, 2025 AT 23:57I hear the hype, but let’s not forget that not every bladder pain stems from muscular issues. Some patients have inflammatory or neuropathic components that won’t respond to PT alone. It’s wise to keep a multimodal approach rather than putting all eggs in one basket.
Emily Torbert
November 2, 2025 AT 19:24Really appreciate how empathetic this post is. It gives hope without making unrealistic promises. The step‑by‑step breakdown feels doable. I’m glad you mentioned tracking progress – that’s a game changer. Thanks for sharing!
Rashi Shetty
November 3, 2025 AT 12:04While the article is well‑written, it could benefit from a more rigorous citation of the studies mentioned. The percentages cited should be tied to peer‑reviewed research to bolster credibility. Additionally, the tone occasionally drifts into promotional language, which may undermine trust. Nonetheless, the practical advice is solid and the inclusion of emojis adds a modern touch. 👍📊
Queen Flipcharts
November 4, 2025 AT 01:57In conclusion, the integration of pelvic‑floor physical therapy into bladder pain management represents a pragmatic, evidence‑informed strategy. It aligns with contemporary principles of minimally invasive care and offers patients a viable path toward improved quality of life.