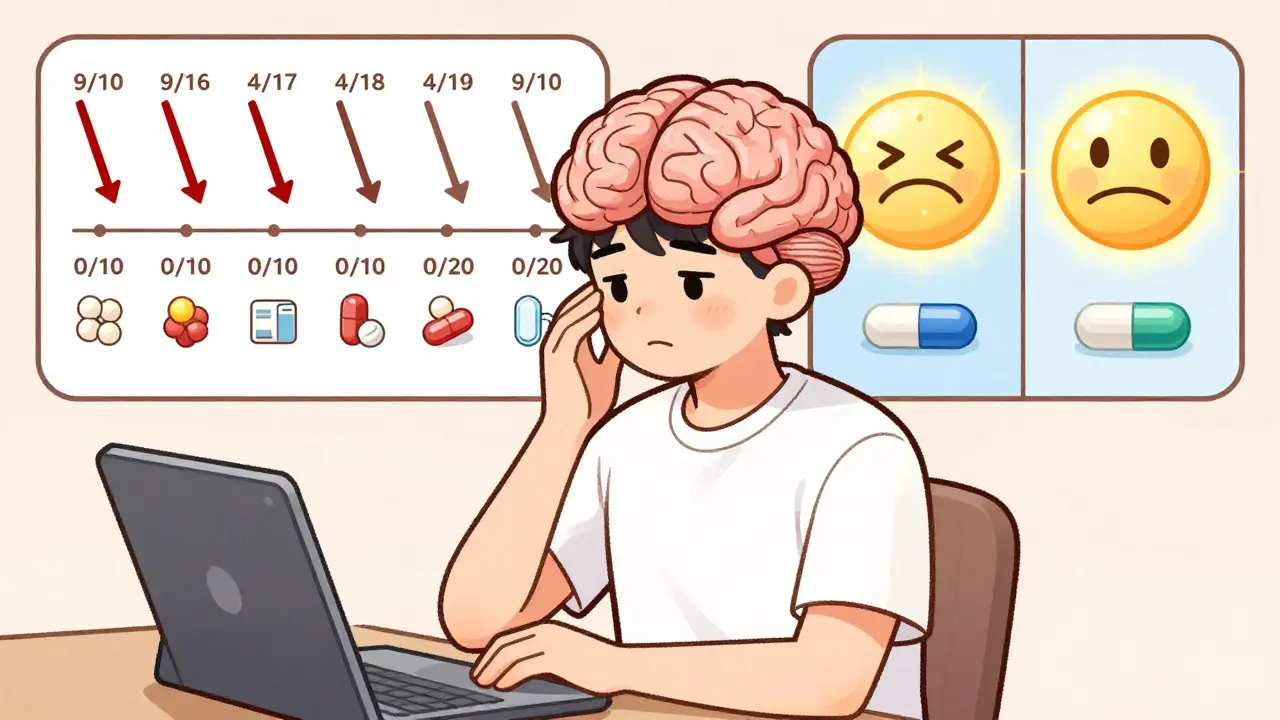
When you switch from a brand-name pill to a generic version, your body doesn’t change - but your brain might. Even if the active ingredient is identical, many people report feeling worse after the switch. Blood pressure climbs. Anxiety returns. Pain comes back. The chemistry hasn’t changed. The difference? Expectation.
Why Generic Pills Feel Less Effective
A 2014 study from the University of Auckland gave people placebo pills labeled as either a well-known brand-name painkiller or a generic version. Both pills were sugar tablets. But those who thought they were taking the brand-name drug reported nearly 40% more pain relief than those who thought they were taking the generic. The only thing different? The label. This isn’t rare. In fact, it’s common. Around 30% of patients believe generic drugs are weaker, even though they’re required by the FDA to be bioequivalent - meaning they deliver the same amount of medicine into your bloodstream at the same rate as the brand version. The FDA allows a 20% variation in absorption (80-125% range), which is still clinically insignificant for nearly all drugs. But perception doesn’t care about statistics. It cares about cost, color, and brand.The Brain’s Role in Drug Response
Your brain doesn’t just passively receive medicine. It actively predicts what’s going to happen. If you’ve been told for years that a blue capsule called "Lipitor" controls cholesterol, your brain learns to expect relief. When you get the same blue capsule labeled "atorvastatin," your brain doesn’t recognize it. And that changes your biology. fMRI scans show that when people believe they’re taking a brand-name drug, their dorsolateral prefrontal cortex - the area tied to expectation and reward - lights up 27% more than when they think they’re taking a generic. That extra brain activity triggers real chemical changes: more endorphins, less stress hormone, better pain control. It’s not imaginary. It’s measurable. And it’s why some people swear their generic antidepressant doesn’t work - even when blood tests show the same drug levels as before.Where the Effect Is Strongest
Not all drugs are affected equally. The placebo effect is strongest with medications you feel immediately - painkillers, antidepressants, and statins. For pain, brand-labeled placebos reduced discomfort by 32.7mm on a 100mm scale. Generic-labeled ones? Only 28.1mm. That’s a gap big enough to make someone quit. For antidepressants, patients on generic sertraline were 22% more likely to stop taking it because they felt "it wasn’t working." In reality, the pills were chemically identical. The same pattern shows up with statins. When patients are told they’re on a generic, they report muscle pain at nearly 4 times the rate of those told they’re on the brand - even when they’re getting a placebo. That’s the nocebo effect: expecting harm makes you feel it.
The Cost-Perception Trap
Here’s one of the weirdest parts: people feel better when they think they’re paying more. In a Harvard study, volunteers received fake painkillers labeled as either $2.50 or $0.10 per pill. The identical pills caused 64% more pain relief when labeled as expensive. Your brain links price to power. It’s evolutionary - we assume expensive things are better. That’s why a $4.83 brand-name pill feels more trustworthy than a $0.08 generic, even if they’re made in the same factory. This isn’t just about individual choice. It’s costing the system billions. In the U.S., unnecessary brand-name prescriptions due to psychological resistance add up to $1.4 billion a year. Medicare plans now track this. Some have started requiring pharmacists to explain bioequivalence when switching patients to generics - and it’s working.How Doctors Can Help
The best way to fix this isn’t to hide the switch. It’s to talk about it. A 2021 study showed that a simple 3-minute conversation cuts nocebo responses by nearly half. What works?- "The FDA requires generic drugs to work the same as brand-name ones. They’re held to the same strict standards."
- "Some people notice a difference in how they feel - not because the medicine is weaker, but because their brain expects something different. That’s normal."
- "Give it two weeks. If you still feel off, we’ll talk. But don’t stop without checking in first."
What Patients Can Do
If you’ve switched and feel worse, don’t assume it’s the drug. Ask yourself:- Did I know I was switching? If you were told, your brain may have already started expecting failure.
- Is the pill a different shape or color? Even small changes can trigger nocebo responses. The FDA now advises manufacturers to keep pill appearance consistent to avoid this.
- Have I given it time? Psychological effects often fade after 10-14 days as your brain adjusts.
Real Stories, Real Results
On Reddit, one user wrote: "My psychiatrist warned me generic sertraline might feel different. I was skeptical - but I tried it anyway. After a week, I felt the same. Now I save $120 a month." Another, on Drugs.com, said: "I switched to generic levothyroxine. My TSH went from 2.1 to 8.7. I went back to brand. My numbers normalized. I don’t care if it’s the same - I feel better on the blue pill." These aren’t lies. They’re real experiences shaped by psychology. The solution isn’t to dismiss them. It’s to understand them.The Future of Generic Prescribing
The FDA is testing a new digital tool - a 12-minute app that walks patients through how generics work. Early results show it reduces nocebo responses by 53%. It’s not magic. It’s education. In Europe, a €2.4 million project is creating standardized patient guides for all 27 EU countries. In the U.S., Medicare plans are now trained to flag high-risk switches - like antidepressants and statins - and offer counseling upfront. The goal isn’t to make people love generics. It’s to make sure they don’t quit them because they think they’re inferior. Because they’re not. They’re the same medicine. Just cheaper. And sometimes, that’s enough.When to Stick With Brand
There are rare cases where switching matters - like thyroid meds (levothyroxine), seizure drugs (phenytoin), or blood thinners (warfarin). Even then, the issue isn’t always bioequivalence. It’s consistency. If you’ve been stable on one brand for years, and your doctor agrees, staying put is fine. But for most people - for high blood pressure, cholesterol, diabetes, depression - generics are just as safe. Just as effective. And if you feel worse after switching? Talk to your provider. Don’t assume the drug failed. Your brain might just need a new story.Do generic drugs work the same as brand-name drugs?
Yes. By law, generic drugs must contain the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also be absorbed into the bloodstream at the same rate and extent, within a narrow FDA-approved range (80-125%). Thousands of studies confirm this. The difference isn’t in the medicine - it’s in the label, the cost, and your expectations.
Why do some people feel worse on generic medication?
It’s often not the drug - it’s the mind. If you believe a generic is weaker, your brain can trigger real physical changes, like increased stress hormones or reduced pain relief. This is called the nocebo effect. Studies show people report more side effects and less improvement when they know they’re on a generic, even if the pill is identical. Changing the pill’s color or size can make this worse.
Is the placebo effect real with generics?
Absolutely. In controlled studies, placebo pills labeled as brand-name drugs produced pain relief equal to real medication. Placebos labeled as generic didn’t. The difference? Only the label. Your brain responds to belief - not just chemistry. This isn’t weakness. It’s how the human nervous system works.
Should I avoid switching to generics because of this?
No - unless your doctor advises otherwise. For most medications, generics are just as safe and effective. If you’re worried, talk to your provider before switching. Ask them to explain bioequivalence. Give it two weeks. Track your symptoms. Most people adjust. The savings - often hundreds a year - are real. And so is the benefit.
Can my doctor help me feel better on generics?
Yes. Doctors who take 3 minutes to explain that generics meet the same FDA standards, acknowledge that perception differences can happen, and encourage a two-week adjustment period see much higher adherence. It’s not about lying - it’s about managing expectations. That’s good medicine.
Are there any drugs where generics really aren’t the same?
For most, no. But in rare cases - like levothyroxine (thyroid), phenytoin (seizures), or warfarin (blood thinning) - even tiny variations in absorption can matter. That’s why doctors sometimes recommend staying on one brand. But even here, many patients switch successfully. The key is consistency: once you’re stable on a generic, don’t switch brands or manufacturers unless necessary.

Angela Spagnolo
December 27, 2025 AT 14:25I switched to generic sertraline last year, and honestly? I was terrified. I thought I'd crash. But I gave it two weeks, tracked my mood daily like the post said... and guess what? I felt the same. No crash. No weirdness. Just saved $110/month. My brain just needed to unlearn the brand-name magic. I'm still weirded out by how powerful expectation is, though.
Sarah Holmes
December 29, 2025 AT 08:10This is a dangerously misleading piece of pseudoscience. You're implying that people who feel worse on generics are merely 'imagining' it - a classic dismissal of real physiological variance. The FDA's 80-125% absorption window is not 'clinically insignificant' for narrow-therapeutic-index drugs. This is not psychology - it's pharmacokinetic variability masked as placebo. You're enabling dangerous cost-cutting at the expense of patient safety.
Jay Ara
December 30, 2025 AT 16:53bro this is so real. i switched my blood pressure med to generic and felt weird for like 3 days. then i just stopped thinking about it and boom - same as before. brain is wild. also saved like 90 bucks a month. india here, generics are the norm, no drama.
Michael Bond
January 1, 2026 AT 10:08Same medicine. Different label. Same result - if you let it be.
Kuldipsinh Rathod
January 2, 2026 AT 03:41my uncle was on generic lisinopril for 5 years. never had a problem. then he switched brands and started feeling dizzy. turned out it was the filler, not the drug. he went back to the original generic and fine again. so yeah, sometimes it's not the brain - it's the pill's coating or dye. but mostly? it's the mind.
SHAKTI BHARDWAJ
January 3, 2026 AT 05:06OMG I KNEW IT. I told my doctor this would happen. I switched to generic levothyroxine and my hair started falling out, i felt like a zombie, my TSH went to 11. I went back to brand and boom - energy, hair, life. This article is trying to gaslight people into taking cheaper poison. I'm not crazy, I'm just not a lab rat.
Matthew Ingersoll
January 3, 2026 AT 15:21The nocebo effect is one of the most underappreciated phenomena in modern medicine. I've seen patients refuse statins because they 'heard generics cause muscle pain' - then, after a placebo-controlled switch with no label, they reported zero side effects. The body follows the narrative. We need to train providers to script this better. It's not just about efficacy - it's about trust.
carissa projo
January 4, 2026 AT 17:53It's fascinating - and heartbreaking - how deeply our minds are wired to equate cost with value, color with potency, and familiarity with safety. We’re not irrational; we’re pattern-seeking primates who evolved to assume expensive things are better. The real tragedy isn't that people feel worse on generics - it's that we've built a system that exploits that instinct to sell overpriced pills. Imagine if we invested as much in patient education as we do in branding. The savings wouldn't just be financial - they'd be psychological.
josue robert figueroa salazar
January 5, 2026 AT 13:20lol so the answer is just don't tell people they're switching? classic. just keep them in the dark. that's the real solution? no wonder trust in medicine is dying.
david jackson
January 5, 2026 AT 20:49Okay, let’s go full neuroscience here. The dorsolateral prefrontal cortex doesn’t just ‘light up’ - it rewires. Every time you take a pill labeled ‘Lipitor,’ your brain forms a synaptic memory: blue capsule = calm cholesterol. When you swap it for ‘atorvastatin’ - same molecule, different shape, different color - your brain doesn’t recognize the pattern. It triggers a stress response. Cortisol spikes. Endorphins dip. You feel worse. It’s not placebo. It’s predictive coding. Your brain is predicting failure because the visual cues are wrong. That’s why consistency matters - not just in dosage, but in aesthetics. The FDA should mandate that generics match brand pill design. Not for marketing - for neurology.
christian ebongue
January 5, 2026 AT 20:50So... you're saying I'm not lazy, I'm just psychologically manipulated by pill color? cool. thanks for the diagnosis, doctor.
Zina Constantin
January 7, 2026 AT 14:17My mom switched to generic metformin and thought it stopped working. We sat down, talked about the science, gave it two weeks, and tracked her glucose. Same numbers. Same energy. She now tells her friends: 'It’s not the pill - it’s the story you tell yourself.' I’m proud of her.