Side Effect Reporting Calculator
How Your Report Helps
Only 6-10% of actual side effects get reported. This calculator shows how many reports are needed to detect a problem.
"One report might not change anything. But 100? That's a signal."
- Article quote on reporting importance
Results
With 0 reports, we estimate:
This means 1 in 0 people reporting may actually represent 1 in 0 of the population.
Why This Matters
According to the article: "Experts estimate only 6% to 10% of actual side effects are ever reported."
A popular antidepressant received a black box warning after post-market data showed increased suicide risk in teens. This was detected through patient reports.
When a new drug or medical device hits the market, it’s easy to assume it’s been thoroughly tested and proven safe. But clinical trials only involve a few thousand people - often healthy volunteers or those with a single condition. Real life? That’s millions of people with different genetics, diets, other medications, chronic illnesses, and lifestyles. That’s where post-market surveillance comes in. It’s not a backup plan. It’s the most important safety net there is.
Why Clinical Trials Aren’t Enough
Before a drug gets approved, it goes through phases of testing. Phase 1 checks for safety in 20-100 people. Phase 2 looks at effectiveness in a few hundred. Phase 3 might involve 1,000-5,000 patients. Sounds solid, right? But here’s the catch: rare side effects - the kind that happen in 1 out of 5,000 or 1 out of 10,000 people - simply won’t show up. And what about someone who’s 82, has kidney disease, takes six other pills, and sleeps poorly? They weren’t in the trial. Yet they’re the ones who’ll be using the drug the most. The same goes for medical devices. A pacemaker might work perfectly in a controlled lab. But in the real world, a patient might sleep on it wrong, clean it with the wrong solution, or have tissue grow around it over time. These problems don’t show up in six-month trials. They show up after five years.How Side Effects Actually Get Found
There’s no magic system. It’s messy, human, and relies on people noticing something’s off and speaking up. The most common way? Spontaneous reporting. In the U.S., the FDA runs MedWatch. Doctors, nurses, pharmacists, and even patients can submit reports when they see something unusual - like a sudden rash, unexplained fatigue, or a device malfunction. In Europe, it’s EudraVigilance. These systems collect hundreds of thousands of reports every year. But here’s the hard truth: experts estimate only 6% to 10% of actual side effects are ever reported. Many doctors don’t have time. Many patients don’t know how. That’s why smarter systems are rising. The FDA’s Sentinel Initiative uses data from over 300 million Americans - electronic health records, insurance claims, pharmacy logs. It doesn’t wait for someone to report a problem. It scans for patterns. If a new blood thinner suddenly shows up in 500 emergency room visits for internal bleeding across three states, the system flags it. No human had to notice. The data did. For medical devices, the EU’s Medical Device Regulation (MDR) requires manufacturers to run Post-Market Clinical Follow-up (PMCF) studies. That means they can’t just sell the device and walk away. They have to track real patients over time. If a new type of hip implant starts breaking at a higher rate than expected after three years, the company must investigate - and tell regulators.The Role of Real-World Evidence
Real-world evidence isn’t a buzzword. It’s the only way to see how drugs and devices behave outside the lab. Think of it like this: clinical trials are like test-driving a car on a closed track. Post-market surveillance is watching how it holds up on icy roads, in traffic jams, with different drivers, over 10 years. AI is making this faster. Companies now use algorithms to scan social media, patient forums, and even online reviews. A spike in posts saying “this new diabetes pill made me dizzy” can trigger an investigation. Oracle Health reported a 40% faster detection rate using AI compared to traditional methods. That’s not science fiction. It’s happening now. But it’s not perfect. False alarms are common. A drug might be linked to headaches - but maybe everyone taking it is stressed out from their illness. That’s why experts don’t act on one report. They look for clusters, timing, and biological plausibility. Did the symptom appear after starting the drug? Did it go away when they stopped? Is there a known mechanism? Only then do regulators take action.
Who’s Responsible?
It’s not just the FDA or EMA. The law puts the burden on manufacturers. If you make a drug or device, you’re legally required to monitor it after it’s sold. In the EU, under MDR, you need a full Post-Market Surveillance Plan, a PMS Report updated yearly, and a system to handle complaints, analyze trends, and report serious incidents. Failure? Fines, recalls, or worse - your product gets pulled. In the U.S., the FDA can require post-approval studies - but only about 29% of these are completed on time, according to Yale research. Delays of over three years are common. That’s a gap in safety. Patients are using the product while regulators wait for data. Healthcare workers are on the front lines. A cardiologist in Boston reported a strange rash from a new anticoagulant - but never heard back. That’s not unusual. Reporting systems are often slow, impersonal, and don’t give feedback. That discourages future reports. And when doctors stop reporting, the system breaks.What Happens When Something’s Found?
Finding a side effect is only step one. What happens next? Sometimes, it’s simple: a label update. The drug’s package insert gets a new warning: “May cause severe liver injury in patients with pre-existing conditions.” Sometimes, it’s more serious. The FDA issued a black box warning - the strongest - for a popular antidepressant after post-market data showed increased suicide risk in teens. That changed prescribing habits overnight. For devices, recalls happen. A 2023 analysis found 55% of Class I recalls (the most serious) were due to problems only found after the product was already in use. One manufacturer had to recall 200,000 insulin pumps because a software bug caused incorrect dosing - a flaw no lab test caught. The goal isn’t to punish. It’s to protect. If a product’s risks outweigh its benefits, it gets restricted or removed. That’s how post-market surveillance saves lives.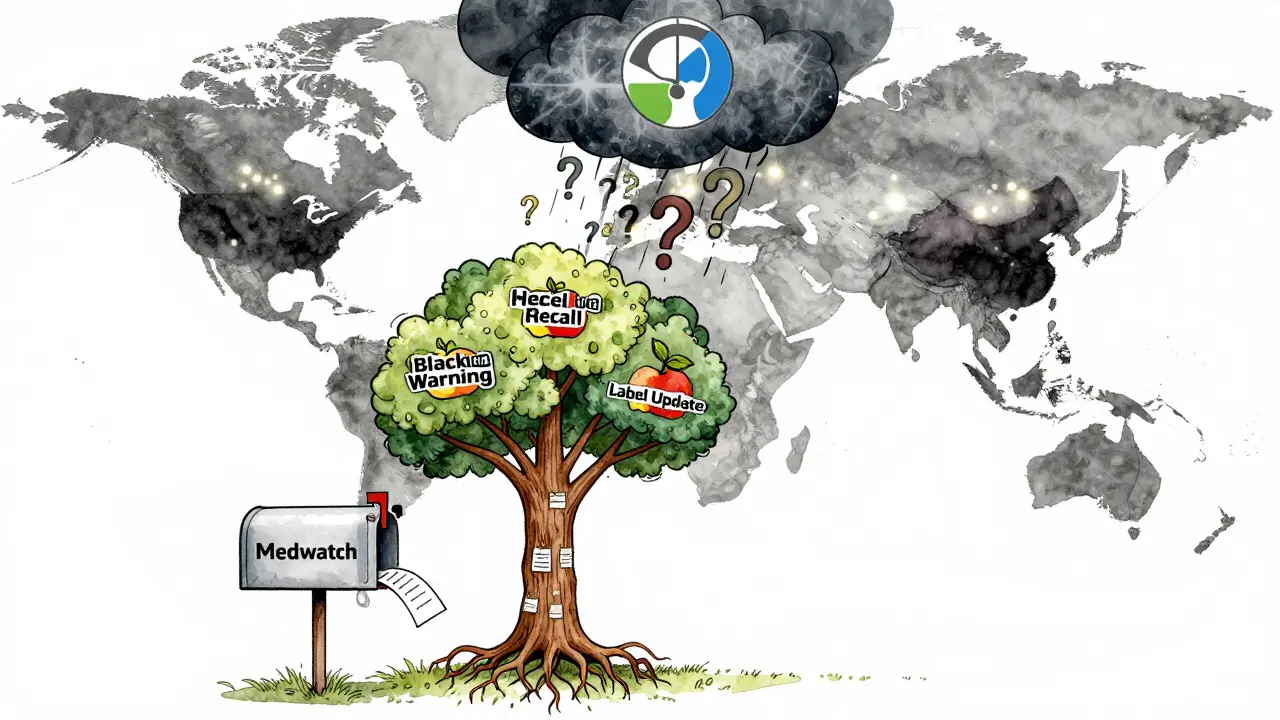
Challenges and Gaps
The system works - but it’s strained. Low- and middle-income countries? Only 28% have functional pharmacovigilance systems. People there often don’t know how to report, or have no way to do it. That’s a global blind spot. New therapies are making things harder. Cell and gene therapies can have effects that show up years later. AI-powered diagnostics? We don’t yet know how to monitor their long-term safety. The tools we have were built for pills and pacemakers, not personalized treatments. And then there’s the human factor. Manufacturers say the EU MDR rules doubled their workload without more staff. Nurses say they’re too busy to file reports. Patients don’t know MedWatch exists. Only 12% of people surveyed in a Johns Hopkins study had ever heard of it.What You Can Do
You don’t have to be a doctor to help. If you take a new medication and feel something strange - a new rash, dizziness, mood changes - write it down. Note the date, the dose, and how long it lasted. Then report it. In the U.S., go to MedWatch (yes, it’s online). In the EU, ask your pharmacist or doctor to help you report. You don’t need to be certain it’s the drug. If you’re worried, report it. One report might not change anything. But 100? That’s a signal. If you use a medical device - a glucose monitor, a knee implant, a breathing machine - pay attention. Does it feel different? Does it beep weirdly? Does the skin around it get red? Tell your provider. Ask them to report it. Don’t assume it’s just you.What’s Next?
The future of safety is faster, smarter, and more connected. Real-time data from wearables. Blockchain to securely share reports across countries. Patient apps that auto-report symptoms. The goal is to catch problems before they become epidemics. But technology alone won’t fix it. We need more doctors trained in pharmacovigilance. We need better tools for patients. We need regulators who act quickly. And we need people - real people - to speak up when something’s wrong. Post-market surveillance isn’t glamorous. It doesn’t make headlines. But every time a dangerous drug is pulled or a faulty device is fixed, it’s because someone noticed, reported, and refused to look away.What is the main purpose of post-market surveillance?
The main purpose is to detect side effects and safety issues that weren’t visible during clinical trials. These include rare reactions, long-term effects, and problems that only appear when a product is used by millions of people with different health conditions, ages, and lifestyles.
How do regulators find out about side effects after a drug is approved?
They use multiple methods: spontaneous reports from doctors and patients (like the FDA’s MedWatch), analysis of electronic health records and insurance claims (like the FDA’s Sentinel Initiative), patient registries, and even AI scanning of social media and online forums. For medical devices, manufacturers are required to run ongoing clinical follow-up studies.
Why are so many side effects never reported?
Doctors are often too busy, patients don’t know how or where to report, and many don’t realize their symptoms could be linked to a medication or device. Studies show only 6-10% of actual adverse events are reported. That means the system is missing most of the data.
Can post-market surveillance prevent dangerous drugs from staying on the market?
Yes. Many drugs and devices have been restricted or pulled because of post-market findings. For example, a popular antidepressant received a black box warning for increased suicide risk in teens after real-world data showed the pattern. Insulin pumps, hip implants, and blood thinners have all been recalled based on post-market signals.
What’s the difference between pharmacovigilance and post-market surveillance?
Pharmacovigilance is the specific term for monitoring drug safety - collecting and analyzing adverse drug reactions. Post-market surveillance is the broader term that includes pharmacovigilance for drugs and also covers medical devices, using methods like clinical follow-up studies and device incident reporting.
Are new technologies making post-market surveillance better?
Yes. AI can now scan millions of electronic health records and social media posts to detect safety signals in days, not years. Wearables and patient apps are starting to provide real-time symptom data. But these tools still rely on human input and proper regulation to be effective.
What should I do if I think a medication caused a side effect?
Write down what happened, when, and how long it lasted. Then report it - even if you’re unsure. In the U.S., go to MedWatch online. In other countries, ask your doctor or pharmacist. Your report could help prevent harm to others.


Priscilla Kraft
January 12, 2026 AT 07:55Just reported my weird dizziness after starting that new blood pressure med 🤓️-took 2 mins on MedWatch. If everyone did this, we’d catch stuff way faster. Seriously, your weird symptom might be someone else’s lifesaver.
Sam Davies
January 12, 2026 AT 12:02Oh wow, a whole article about how the system is broken and nobody cares. Groundbreaking. Next you’ll tell me water is wet and the FDA has a budget problem. Meanwhile, my GP still thinks ‘side effect’ is a four-letter word. 🙃
Christian Basel
January 13, 2026 AT 21:14Post-market surveillance is essentially a reactive pharmacovigilance framework predicated on spontaneous adverse event reporting, which suffers from severe underreporting bias due to cognitive load and systemic inertia. The sentinel initiative mitigates this via distributed data lakes, but the signal-to-noise ratio remains suboptimal without NLP-enhanced phenotyping. Also, manufacturers are incentivized to delay PMCF. It’s a mess.
Jennifer Littler
January 14, 2026 AT 14:57As a clinical pharmacist, I’ve seen this up close. We get zero feedback after reporting. One time I flagged a combo drug causing hallucinations in elderly patients. Nothing. No call, no email, no update. So now I just sigh and move on. If the system doesn’t acknowledge you, why bother?
And don’t get me started on how device reps ghost patients after sale. ‘Just call your doctor’ isn’t a plan.
Jason Shriner
January 16, 2026 AT 13:48So… we’re trusting our lives to algorithms that scan Reddit and Instagram for typos? Next thing you know, some AI will pull metformin because someone said ‘I feel weird after taking it while on a keto diet’ and 12 other people liked it. This isn’t science. It’s TikTok medicine.
Also, I’m pretty sure the ‘black box warning’ is just the FDA’s way of saying ‘we’re too lazy to fix this, so here’s a sticker.’
Alfred Schmidt
January 18, 2026 AT 04:24STOP. JUST STOP. I had a pacemaker implanted last year. Three months later, it started buzzing like a dying bee. I called my doctor. He said, ‘That’s normal.’ I called again. He said, ‘It’s probably anxiety.’ I went to the ER. They found a loose lead. I almost died because NO ONE LISTENS. YOU THINK THIS IS ABOUT REPORTING? IT’S ABOUT PEOPLE BEING HEARD.
And yeah, I’m mad. I’m FURIOUS. And I’m not alone.
Sean Feng
January 20, 2026 AT 03:23Doctors don’t report because they’re overworked. Patients don’t report because they don’t know how. Regulators don’t act because they’re slow. Manufacturers don’t care because they’re rich. We’re all just waiting for the next scandal. Classic.
Vincent Clarizio
January 21, 2026 AT 20:35Think about it. We put a man on the moon in 1969. We’ve mapped the human genome. We can predict the weather two weeks out. But we still can’t reliably track whether a pill causes a rash in 1 in 10,000 people? That’s not a failure of technology. That’s a failure of will. We prioritize profit over people. The system isn’t broken-it was designed this way. Every delay, every ignored report, every ‘we’ll look into it’ is a quiet vote for corporate over compassion. And we’re all complicit because we scroll past the warning labels and keep clicking ‘accept’.
It’s not about MedWatch. It’s about whether we believe human life is worth more than quarterly earnings.
When your grandma’s new heart drug causes internal bleeding and the company says ‘rare, but possible,’ who do you think they’re really talking to? Not you. Not me. Someone they’ll never meet. And that’s the real tragedy.
We don’t need more AI. We need more accountability. More transparency. More courage. Not just from regulators. From us.
So yeah, report your dizziness. But also demand better. Because if we keep treating safety like an afterthought, we’re not just failing patients-we’re failing our own humanity.
Alex Smith
January 22, 2026 AT 22:10Love how you mentioned AI scanning social media. But here’s the kicker-most patients don’t post about side effects because they’re scared they’ll be called ‘drug seekers’ or ‘hysterical.’ So the data we get is skewed toward loud, angry voices. The quiet ones? The ones who just feel off and go to bed? They vanish. We need systems that reach out, not just scan.
Also, can we make a simple app? One tap: ‘I feel weird after taking X.’ Auto-send to FDA. No forms. No jargon. Just ‘I’m not okay.’ That’s all it takes.
Adewumi Gbotemi
January 23, 2026 AT 15:32Here in Nigeria, we have no system. If you get sick from a drug, you go to the market and buy another. No one reports. No one knows. We need help. Not just words.
Priya Patel
January 25, 2026 AT 12:07My mom took that new diabetes pill and got dizzy for 3 weeks. We thought it was aging. Then I read this and reported it. Two weeks later, the FDA sent a notice about the same issue. I cried. I didn’t think anyone would care. Turns out, someone did.
So yeah. Report. Even if you think it’s nothing. It’s not nothing.
Priscilla Kraft
January 25, 2026 AT 15:27@6733 I’m so glad you reported it. That’s exactly how change starts. One person. One report. One life saved. 🙌💖