What PSA Testing Really Tells You (and What It Doesn’t)
PSA testing is the most common way men get screened for prostate cancer. It’s a simple blood test that measures prostate-specific antigen, a protein made by the prostate gland. But here’s the thing: PSA doesn’t diagnose cancer. It just signals that something might be off. A high PSA level could mean cancer, but it could also mean an enlarged prostate, an infection, recent ejaculation, or even a hard bike ride.
The test became popular after the FDA approved it for screening in 1994. Since then, millions of men have had it done. But the numbers don’t lie: only about 1 in 4 men with a high PSA actually have prostate cancer. That means 3 out of 4 men who get called back for a biopsy are told they’re cancer-free. And that’s not just frustrating-it’s stressful. Studies show nearly 4 in 10 men who go through an unnecessary biopsy report lasting anxiety, sometimes for over half a year.
For years, doctors used a cutoff of 4.0 ng/mL to decide who needed a biopsy. Now, many guidelines, including the National Comprehensive Cancer Network, have lowered that to 3.0 ng/mL. Why? Because research shows cancer risk starts rising even below 4.0. But lowering the bar means more false alarms. A 2023 study found that switching from 4.0 to 3.0 ng/mL increased the number of Black men referred for biopsy by 66%, even though their actual cancer detection rate was lower than in White men. That’s a real disparity with real consequences.
Age matters too. A PSA of 5.0 might be normal for a 70-year-old but worrying for a 50-year-old. Still, there’s no universal agreement on age-adjusted ranges. Some doctors use them. Others don’t. And the evidence behind them isn’t strong. The bottom line? A single PSA number doesn’t tell you much. What matters more is how it changes over time-and whether you’ve had other tests to back it up.
When PSA Is High: What Happens Next?
If your PSA is elevated, your doctor won’t rush you into a biopsy. Good ones will look at your history first. Did you have a prostate infection last month? Did you ride a bike yesterday? Did you have sex the night before? These things can spike PSA temporarily. That’s why many experts recommend repeating the test before jumping to the next step.
For men with PSA between 3 and 10 ng/mL, the Stockholm3 trial showed that repeating the test over time, instead of rushing to biopsy, reduced unnecessary procedures by nearly 17%. That’s a big win. But not all doctors do this. Many still follow the old playbook: PSA up → biopsy.
That’s where newer tests come in. The Prostate Health Index (PHI) and 4Kscore are blood tests that look at different forms of PSA and other proteins. They’re better than the standard PSA test at telling the difference between harmless enlargement and aggressive cancer. One study found they outperformed the old free-to-total PSA ratio in men with PSA levels between 2 and 10 ng/mL. These tests can help you avoid a biopsy if you’re low risk. But they cost $300-$450, and insurance doesn’t always cover them. Medicare does, but you’ll often need prior authorization.
Another option is an MRI of the prostate. Multiparametric MRI can spot suspicious areas without cutting into tissue. When combined with PSA results, it’s far more accurate than PSA alone. A 2023 review found that MRI alone had a 72% negative predictive value-meaning if it’s clean, there’s a 72% chance you don’t have dangerous cancer. But when you combine MRI with PSA and biomarker tests, that number jumps to 91%. That’s powerful. And it’s changing how screening works.
The Biopsy: What to Expect and Why It’s Still Necessary
If your PSA is high and your MRI shows something suspicious, or if you’re in a higher-risk group, your doctor will likely recommend a biopsy. This is when a needle pulls tiny tissue samples from your prostate. It’s done through the rectum (transrectal) or between the scrotum and anus (transperineal). Local anesthesia is used, but it’s still uncomfortable. You’ll feel pressure, maybe a pinch. Most men describe it as brief but unpleasant.
Biopsies aren’t perfect either. They can miss cancer if the samples don’t hit the right spot. They can also cause bleeding, infection, or urinary issues afterward. About 1 in 20 men need antibiotics after a biopsy. And if you’re on blood thinners, you’ll need to stop them first-adding another layer of complexity.
But here’s the truth: even with better screening tools, a biopsy is still the only way to confirm cancer. No blood test or scan can say for sure whether cells are malignant. That’s why, despite its flaws, it remains the gold standard. The goal now isn’t to avoid biopsy altogether-it’s to avoid unnecessary ones. That’s why combining MRI with biomarker tests is becoming the new standard of care. If your MRI looks clean and your PHI score is low, you might be able to delay or skip the biopsy entirely.
Treatment Options: Not Every Cancer Needs Immediate Action
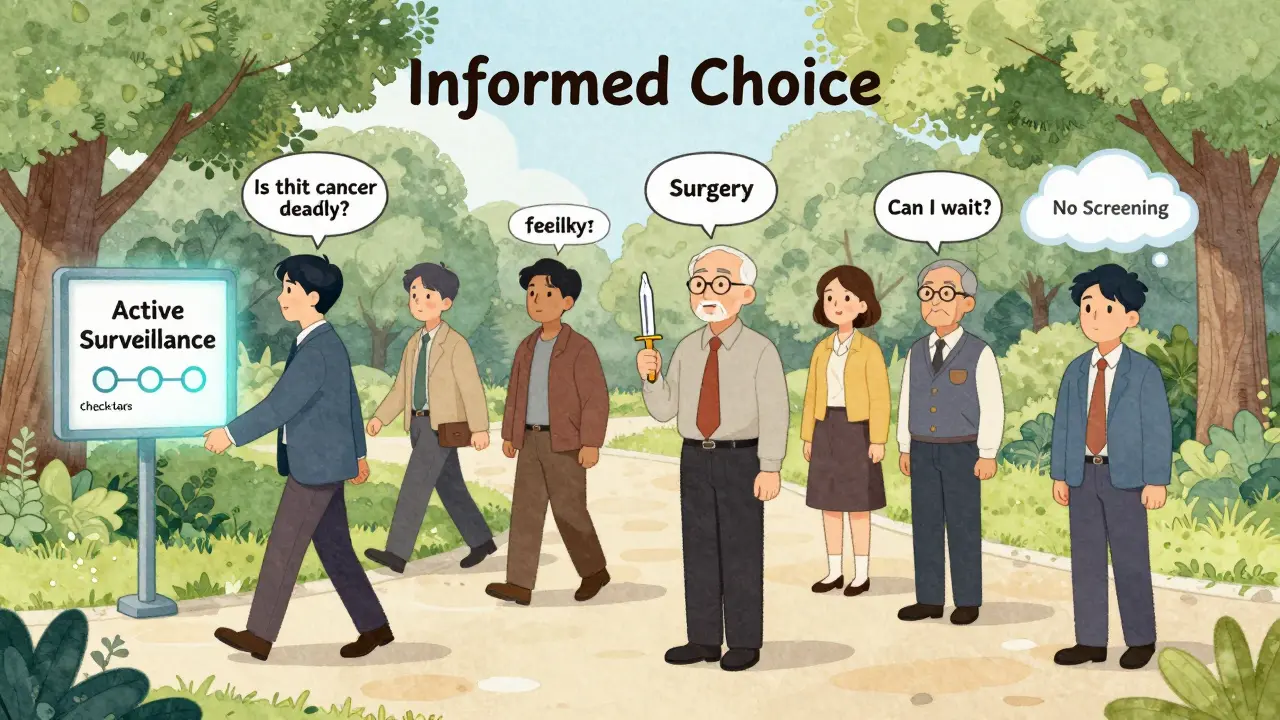
Once cancer is confirmed, the next question isn’t always “What’s the best treatment?” It’s “Does this cancer even need treatment?”
Prostate cancer grows slowly in many men. In fact, autopsies show that up to 40% of men over 70 have prostate cancer they never knew about-and never died from. That’s why active surveillance is now a mainstream option for low-risk cancers. Instead of surgery or radiation right away, you get regular PSA tests, MRIs, and repeat biopsies to watch for changes. If the cancer stays quiet, you don’t need treatment. If it starts growing, you can step in.
Active surveillance works best for men with low-grade tumors (Gleason score 6 or Grade Group 1), small amounts of cancer in the biopsy, and no symptoms. Studies show that over 80% of men on active surveillance avoid treatment for at least 10 years. And their survival rates are the same as those who get immediate surgery.
For men who do need treatment, options include:
- Radical prostatectomy: Surgery to remove the prostate. It’s effective but can cause incontinence or erectile dysfunction in up to 30% of men, depending on age and nerve-sparing technique.
- External beam radiation: High-energy beams target the prostate. Side effects include bowel irritation, urinary urgency, and fatigue. It’s often used for men who aren’t good surgery candidates.
- Brachytherapy: Radioactive seeds are implanted directly into the prostate. Less invasive than surgery but can cause urinary blockage.
- Focal therapy: Newer, less common. Targets only the tumor area, sparing healthy tissue. Still being studied, but promising for select cases.
There’s no one-size-fits-all. Your choice depends on your age, overall health, cancer grade, and personal priorities. A 65-year-old with a high-risk tumor might choose surgery. A 75-year-old with low-grade cancer might choose surveillance. Neither is wrong.
Who Should Get Screened-and When?
There’s no universal rule. The U.S. Preventive Services Task Force says men aged 55 to 69 should decide for themselves after talking to their doctor. For men at higher risk-Black men, or those with a father or brother who had prostate cancer-screening should start at 45. Some experts recommend a baseline PSA at age 40 to set a personal reference point.
Men over 70 rarely benefit from screening. The risks of overdiagnosis and treatment side effects usually outweigh the benefits. Unless you’re in excellent health and have a life expectancy of 15+ years, screening isn’t recommended.
What’s missing from most conversations? Counseling. The American Urological Association says a proper screening discussion should take 15 to 20 minutes. That means talking about: the chance of finding cancer, the risk of false positives, the likelihood of unnecessary treatment, and the possible side effects. Most primary care doctors don’t have time for this. That’s why men often get screened without truly understanding what they’re signing up for.
The Future: Better Tools, Smarter Decisions
The field is changing fast. The IsoPSA test, which looks at the shape of PSA molecules instead of just the amount, showed 92% sensitivity and 95% specificity in recent trials. That’s better than any current blood test. AI is also being trained to spot patterns in PSA trends over time, potentially replacing fixed cutoffs altogether.
And then there’s the PICTURE trial-still ongoing-testing whether starting with an MRI instead of a PSA test can cut unnecessary biopsies by half. Early results suggest it can. If it pans out, we may see a future where men get an MRI first, and only those with suspicious findings go on to PSA testing and biopsy.
For now, the best approach is layered: start with a baseline PSA at 40-45. If it’s low, wait five years. If it’s higher, repeat it. Then add a biomarker test like PHI or 4Kscore if needed. If anything looks off, get an MRI. Only then, if the MRI is suspicious, consider a biopsy. This step-by-step strategy reduces false alarms, cuts down on unnecessary procedures, and still catches dangerous cancers early.
What This Means for You
If you’re a man over 45, don’t wait for your doctor to bring up PSA testing. Ask for it. But don’t stop there. Ask what your PSA number means in context. Ask if you’re a candidate for a PHI or 4Kscore test. Ask if an MRI makes sense. Ask about active surveillance if cancer is found.
Prostate cancer screening isn’t about finding cancer at all costs. It’s about finding the right cancer-the kind that could kill you-and avoiding the kind that won’t. The tools are better than they were ten years ago. But the decision still rests on you. And that’s why understanding the numbers, the risks, and the alternatives isn’t just helpful-it’s essential.