What Is Retinal Vein Occlusion?
Retinal vein occlusion (RVO) happens when a vein in the retina gets blocked, stopping blood from flowing out. This causes fluid and blood to leak into the retina, leading to swelling and vision loss. It’s not painful, but the vision loss can come on suddenly-sometimes just a blur, sometimes almost total blindness in one eye.
There are two main types: central retinal vein occlusion (CRVO), which blocks the main vein, and branch retinal vein occlusion (BRVO), which affects smaller branches. BRVO is more common and often happens where a hard artery crosses over a vein, squeezing it shut. CRVO tends to be more severe and affects vision more broadly.
It’s not rare. Around 16.4 million people worldwide have RVO, and it’s one of the top causes of vision loss in people over 50. The good news? Treatment today can help many people regain sight-if they get care early.
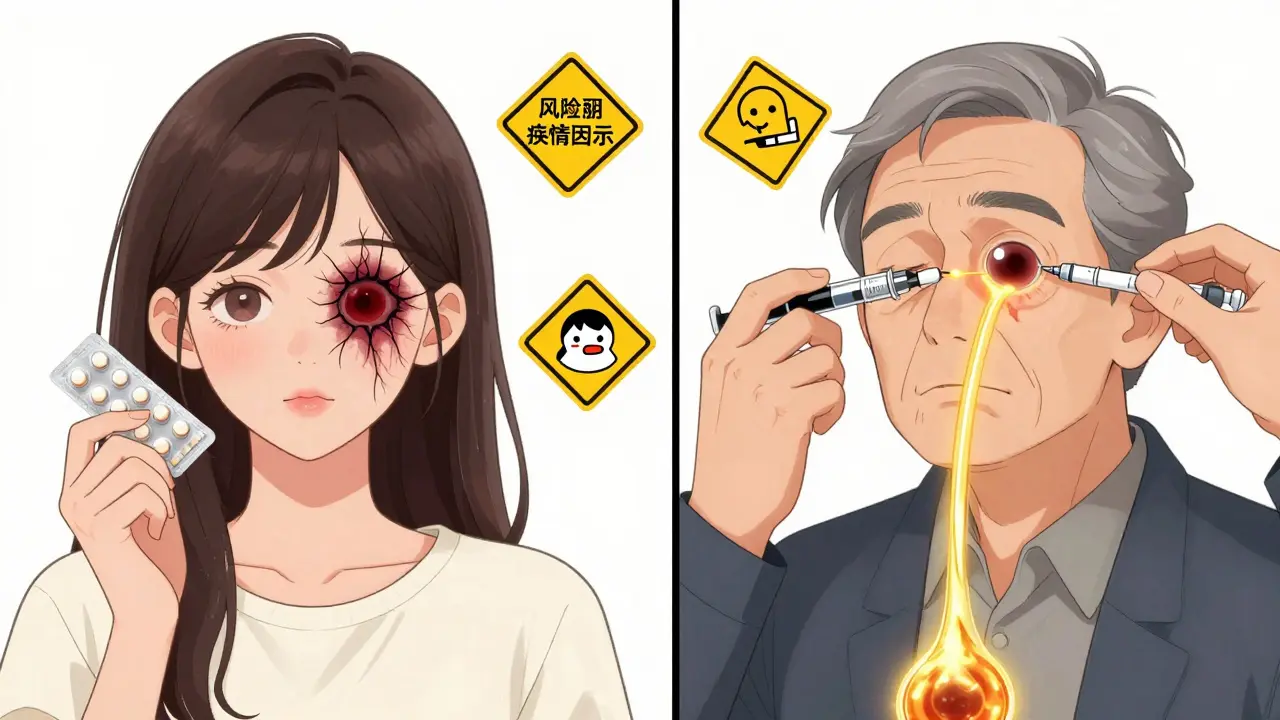
Who’s at Risk for Retinal Vein Occlusion?
Age is the biggest risk factor. More than 90% of CRVO cases happen in people over 55, and over half of all RVO cases occur in those 65 and older. But it’s not just an older person’s disease. About 5-10% of cases strike people under 45, and those cases often have different causes.
The most common health issue tied to RVO is high blood pressure. Up to 73% of CRVO patients over 50 have it, and even younger patients with RVO are far more likely to have uncontrolled hypertension. Diabetes also plays a role, affecting about 10% of RVO patients over 50, though it’s rare in younger cases. High cholesterol is another big one-about 35% of people with RVO have total cholesterol above 6.5 mmol/L.
Glaucoma, especially when eye pressure is high, increases risk too. That’s because pressure on the optic nerve can compress the vein where it exits the eye. Smoking doubles your risk, and being overweight or inactive adds to the problem. Hardened arteries (atherosclerosis) are the root cause in most cases, so anything that speeds that up-smoking, poor diet, inactivity-makes RVO more likely.
For women under 45, birth control pills are a known trigger, especially for CRVO. Blood disorders like polycythemia vera, multiple myeloma, or inherited clotting conditions like factor V Leiden also show up more often in younger patients. If you’re under 45 and get RVO, your doctor will likely check for these hidden causes.
How Are RVO Injections Used to Treat Vision Loss?
There’s no quick fix to unblock the vein. Instead, treatment focuses on the damage it causes-mainly macular edema, which is fluid buildup in the center of the retina. That’s what blurs your vision.
The go-to treatment is injections directly into the eye. Two types are used: anti-VEGF drugs and corticosteroids.
Anti-VEGF drugs like ranibizumab (Lucentis), aflibercept (Eylea), and bevacizumab (Avastin) block a protein called VEGF that causes leaking blood vessels. Clinical trials show these can improve vision by 15-18 letters on an eye chart in just six months. That’s often the difference between barely reading a clock and reading a phone screen.
Bevacizumab isn’t officially approved for the eye, but it’s used in 60-70% of injections at public hospitals because it costs about $50 per dose. The brand-name versions cost $2,000 each. That price gap makes a huge difference for patients on fixed incomes.
Corticosteroid injections, like the dexamethasone implant (Ozurdex), work differently. They reduce inflammation and swelling. In one study, 27.7% of CRVO patients gained 15 or more letters of vision after six months with Ozurdex-compared to just 12.9% with a placebo. But steroids come with risks: about 60-70% of patients develop cataracts, and 30% get higher eye pressure that needs medication.
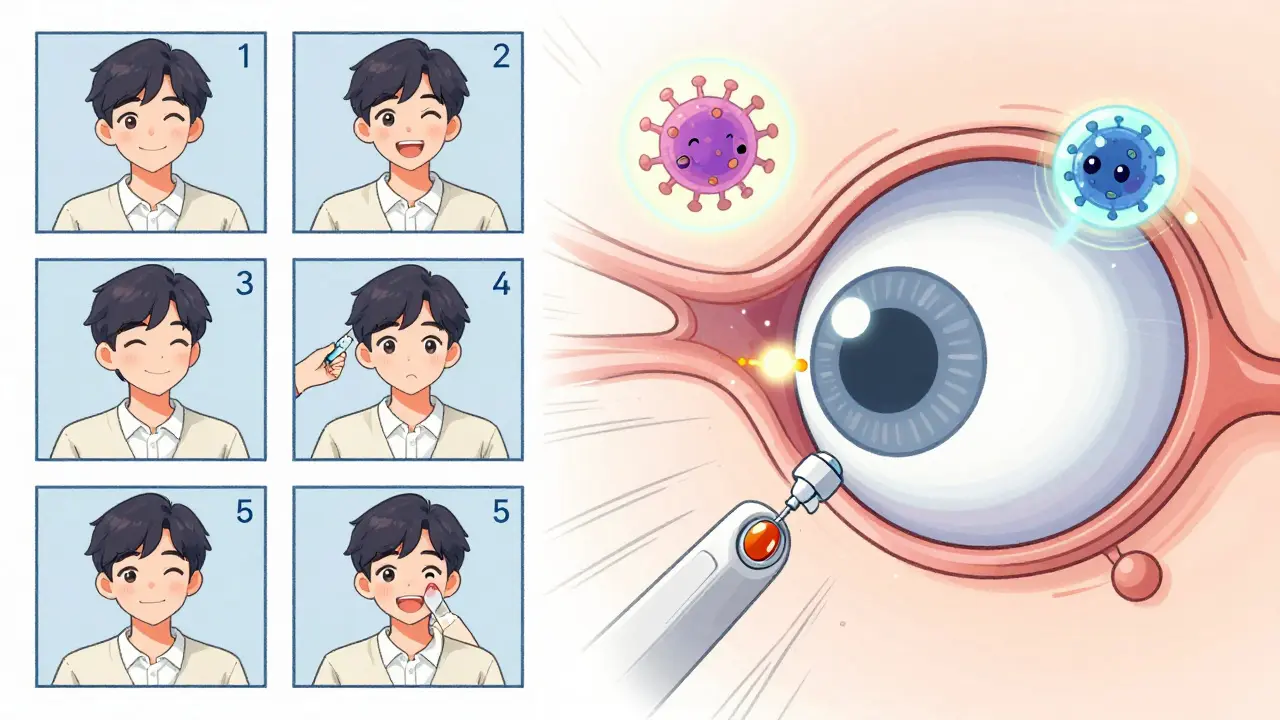
What Does the Treatment Process Look Like?
Before any injection, your eye doctor will do a full exam. That includes checking your vision, looking at the retina with a special lens, and taking detailed scans with optical coherence tomography (OCT). OCT measures the thickness of the retina. If it’s over 300 micrometers, treatment usually starts.
The injection itself takes 5-7 minutes. Your eye is numbed with drops, cleaned with antiseptic, and held open with a tiny clip. You might feel pressure, but not sharp pain. Afterward, you might see floaters or have a red spot on the white of your eye-both are normal and fade quickly.
Most patients start with monthly injections. After a few months, if the swelling goes down, the doctor may switch to a treat-and-extend plan: you get an injection, then wait 6 weeks, then 8, then 10-only coming back if swelling comes back. This reduces the number of shots per year from 12 to 8 or fewer.
Real-world data shows that patients who stick with treatment for a year often see their vision improve from 20/200 to 20/60 or better. That’s the difference between seeing shapes and reading street signs.
Why Do Some People Not Respond to Injections?
Not everyone improves. About 20-30% of patients don’t gain much vision after several anti-VEGF shots. That’s often because the swelling is too advanced, or the vein blockage is too severe.
Doctors now look at other factors to predict who will respond. Patients with very poor baseline vision (worse than 20/200) often do better with steroid implants first. Those with better starting vision usually get better results with anti-VEGF drugs. Some patients switch from one type to the other after 6 months if there’s no improvement.
There’s also a group called treatment fatigue-people who get so overwhelmed by the monthly visits, the cost, or the anxiety that they stop coming. One patient on a support forum said she missed appointments after 18 months because the fear of injections became worse than the vision loss.
That’s why some clinics now offer counseling, financial aid programs, or even home visits for monitoring. If you’re struggling with the burden, talk to your doctor. There are options.
What’s New in RVO Treatment?
The future of RVO treatment is about reducing how often you need shots. A new device called Susvimo, which slowly releases ranibizumab from an implant in the eye, is already approved for another eye disease and is now being tested for RVO. If it works, patients might only need refills every 6 months instead of monthly.
Gene therapy is also in early trials. One experimental treatment, RGX-314, uses a harmless virus to deliver a gene that makes your eye produce its own anti-VEGF protein. If successful, you might need just one injection that lasts years.
Another promising approach combines two drugs: aflibercept plus OPT-302, which blocks a different VEGF protein. Early results suggest this combo works better than either drug alone for stubborn swelling.
Doctors are also using new OCT scans that show blood flow in the retina-not just swelling. This helps them predict who will respond to treatment before they even start.
What Should You Do After Diagnosis?
First: don’t panic. RVO isn’t a death sentence for vision. With treatment, most people stabilize or improve.
Second: get your overall health in check. Control your blood pressure. Get your cholesterol and blood sugar tested. Quit smoking. Start walking 30 minutes a day. These steps won’t fix the blocked vein, but they prevent more damage and reduce the chance of it happening in your other eye.
Third: stick with the treatment plan. Missing injections is the #1 reason vision doesn’t improve. If cost is an issue, ask about bevacizumab or patient assistance programs. If anxiety is the problem, ask if your clinic offers relaxation techniques or if you can bring someone with you.
Finally: keep your appointments. Even if your vision feels fine, your doctor needs to monitor for new swelling or pressure changes. RVO can lead to glaucoma or retinal detachment later on if not watched.

Michael Bond
December 25, 2025 AT 15:30josue robert figueroa salazar
December 26, 2025 AT 16:32Joanne Smith
December 27, 2025 AT 21:45Jody Kennedy
December 28, 2025 AT 22:40jesse chen
December 30, 2025 AT 12:12Sarah Holmes
December 30, 2025 AT 12:13Alex Ragen
December 31, 2025 AT 05:51christian ebongue
December 31, 2025 AT 16:30Lori Anne Franklin
January 1, 2026 AT 11:06Bryan Woods
January 3, 2026 AT 07:24Matthew Ingersoll
January 3, 2026 AT 23:44