When your doctor prescribes a medication like levothyroxine, warfarin, or tacrolimus, you might assume all versions are the same. But with NTI drugs, that assumption can be dangerous. These aren’t ordinary pills. They’re narrow therapeutic index drugs - meaning the difference between a dose that works and one that harms you is razor-thin. A 5% change in blood concentration could mean your seizure returns, your blood clots, or your transplant gets rejected. So when pharmacies swap your brand-name drug for a cheaper generic, should you let them?
What Makes a Drug an NTI Drug?
NTI stands for Narrow Therapeutic Index. The FDA defines it as drugs where small changes in blood levels can cause serious harm - either treatment failure or life-threatening side effects. Think of it like walking a tightrope. Too little, and the drug doesn’t work. Too much, and you overdose. There’s no middle ground.
Common NTI drugs include:
- Levothyroxine (Synthroid, Tirosint)
- Warfarin (Coumadin)
- Tacrolimus (Prograf)
- Phenytoin (Dilantin)
- Cyclosporine (Neoral, Sandimmune)
- Carbamazepine (Tegretol)
These aren’t rare. Millions of people take them. Levothyroxine alone is prescribed over 30 million times a year in the U.S. And while generics cost 30% to 85% less - sometimes as low as $4 a month versus $60 for brand - the question isn’t just about price. It’s about safety.
How Are Generic NTI Drugs Approved?
The FDA says all generics must be bioequivalent to the brand. That means they must deliver the same amount of drug into your bloodstream within the same timeframe. For most drugs, that’s a range of 80% to 125% of the brand’s levels. But for NTI drugs, the rules changed in 2014.
Now, the FDA uses “scaled bioequivalence.” Instead of a fixed range, the acceptable window shrinks based on how much the brand drug’s levels naturally vary in people. For some NTI drugs, the acceptable range is as tight as 90% to 111%. That’s stricter than almost any other drug category.
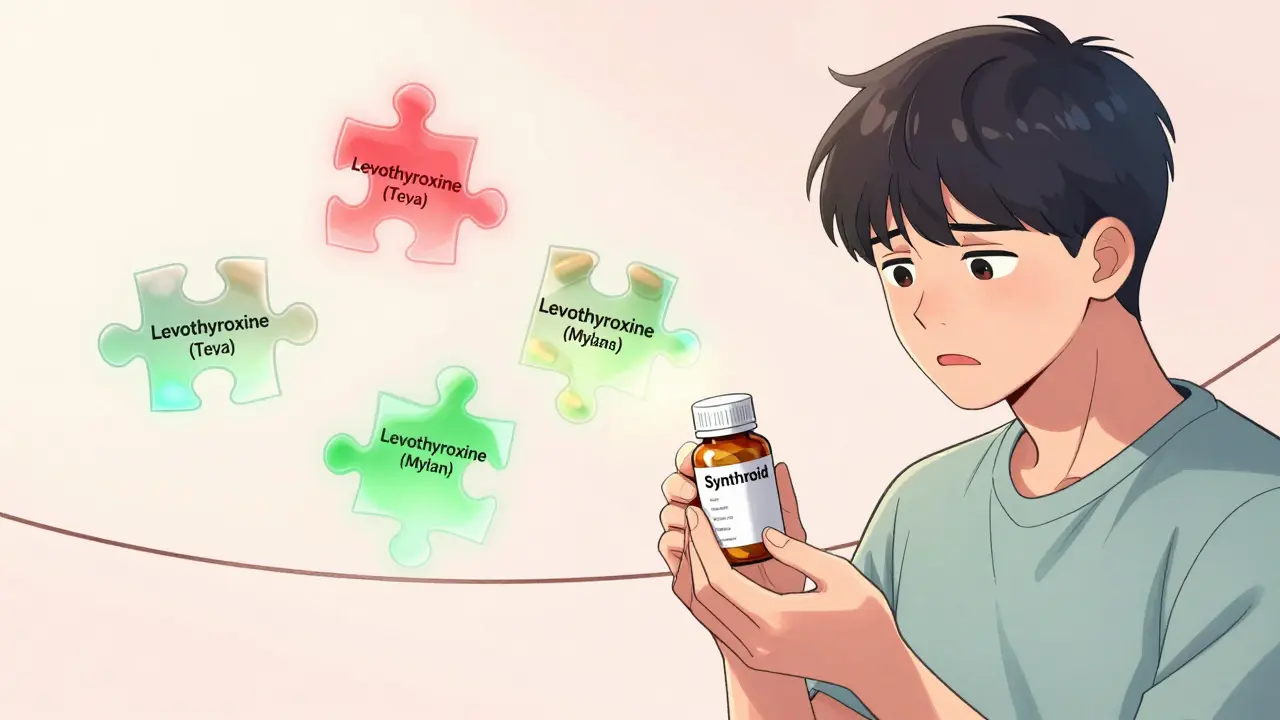
Still, the FDA doesn’t publish an official list of NTI drugs. Experts estimate there are 15 to 20. The Orange Book lists them with an “AB” rating - meaning they’re considered therapeutically equivalent. But here’s the catch: just because a generic is AB-rated doesn’t mean switching between different generic versions is safe.
Real-World Evidence: Do Generics Work?
Studies show mixed results - and that’s the problem.
A 2022 FDA-funded study of nearly 18,000 levothyroxine users found no difference in thyroid hormone levels between those on brand and generic versions. Similar results came from a 3.5-million-patient study on diabetes and hypertension drugs. That sounds reassuring. But those studies didn’t look at patients switching between different generic manufacturers.
When you switch from Synthroid to one generic, then later to another generic, the story changes. A 2022 survey of pharmacists found that 87% believe generic NTI drugs are effective. But 62% admitted they’ve seen patients have problems after switching manufacturers - even if both were AB-rated.
For tacrolimus, transplant patients face real risks. One case study showed a patient’s drug levels dropped 40% after switching generic brands - leading to organ rejection. The fix? Go back to the original brand - or stick with the same generic manufacturer forever.
And for epilepsy? The Epilepsy Foundation’s 2022 survey found 42% of patients reported breakthrough seizures after switching to a generic. While self-reported, these aren’t isolated anecdotes. Clinicians see it in real time.
Who Should Stay on Brand?
There’s no one-size-fits-all answer. But here’s who should think twice before switching:
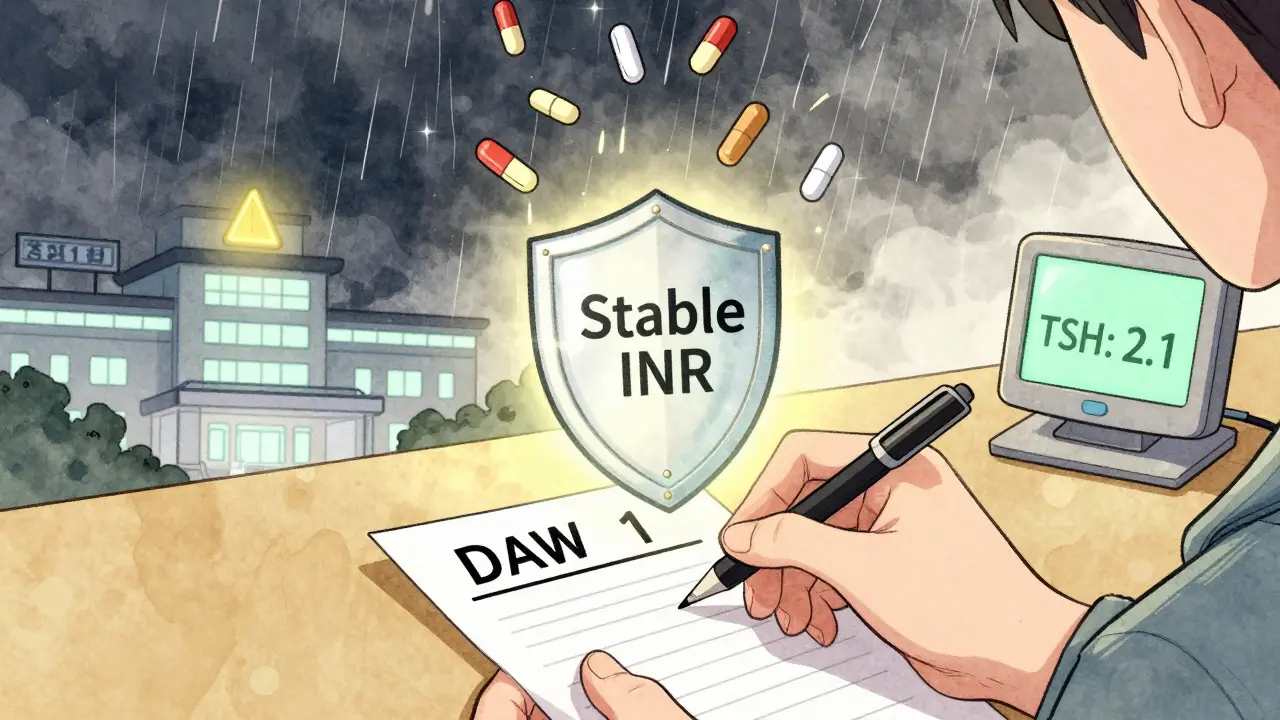
- Patients already stable on brand: If your thyroid levels, INR, or drug concentration have been steady for months - don’t rock the boat. Stability matters more than savings.
- Patients with a history of adverse events: If you’ve ever had a seizure, clot, or rejection after a generic switch, your body may be sensitive to even tiny changes.
- People on multiple NTI drugs: If you’re taking warfarin and tacrolimus together, each switch multiplies your risk.
- Older adults or those with kidney/liver issues: Your body processes drugs slower. Small changes hit harder.
For new patients? Generics are usually fine. Start with the cheapest option. But if your levels don’t stabilize after 4 to 8 weeks, switch back to brand. That’s the standard protocol.
What You Can Do Right Now
You don’t have to guess. Here’s what to do:
- Ask your pharmacist: “Is this the same manufacturer as last time?” If it changed, ask if you can keep the old one.
- Check your prescription label: Generic names often list the manufacturer (e.g., “Levothyroxine (Teva)” or “Warfarin (Mylan)”).
- Request “Dispense as Written”: Tell your doctor you want to stay on the same version. They can write “DAW 1” on the prescription - meaning no substitutions allowed.
- Monitor your levels: If you switch, get blood tests 4 to 8 weeks later. For levothyroxine, that’s TSH. For warfarin, it’s INR. For tacrolimus, it’s whole blood concentration.
- Track symptoms: Write down changes in energy, mood, bruising, tremors, or seizures. Bring it to your next appointment.
Insurance companies are pushing hard for generics. Many now require prior authorization for brand-name NTI drugs. You might have to pay the full price difference - sometimes $40 extra per month. But that’s cheaper than a hospital visit from a drug reaction.
The Bigger Picture: What’s Changing?
The FDA launched the NTI Drug Registry in 2023 to track real-world outcomes. AHRQ is funding a $2.4 million study tracking 50,000 patients through 2025. The goal? To finally answer this question with hard data.
Experts agree on one thing: blanket rules don’t work. Some NTI drugs, like levothyroxine, are likely safe to switch. Others, like phenytoin, still need caution. The future isn’t brand vs. generic - it’s consistent sourcing. Once you find a version that works, stick with it.
Cost matters. But your health matters more. If you’re stable, don’t risk it. If you’re new, try the generic - but monitor closely. And never assume two generics are the same just because they have the same name.

Kegan Powell
January 28, 2026 AT 05:12Man i just switched my levothyroxine to the cheap one last month and my energy dropped like a rock 😅
Thought it was stress or sleep but nope - got my TSH checked and it was way off
Went back to brand and boom - back to normal
Costs more but my brain doesn’t feel like mush anymore
Harry Henderson
January 28, 2026 AT 10:35Stop being cowards. If you can’t handle a $4 pill, you don’t deserve to live in a country with healthcare. Generic equals generic. The FDA says so. End of story. Get over it.
suhail ahmed
January 28, 2026 AT 19:42Bro in India we use generics for everything - thyroxine, warfarin, you name it - and we’re fine
But here’s the twist: we stick to ONE brand forever once we find it
Not because it’s expensive - because consistency is king
Switching between Indian generics? Yeah that’s when things go sideways
So it’s not brand vs generic - it’s same generic vs new generic
Candice Hartley
January 30, 2026 AT 08:25My mom switched to generic tacrolimus after transplant and started having tremors
She didn’t say anything for weeks until she almost fell down the stairs
Thank god they caught it in time
Don’t ignore the little signs - they’re screaming
Andrew Clausen
January 30, 2026 AT 11:13The FDA's 'scaled bioequivalence' is a statistical illusion designed to appease pharmaceutical lobbying groups. The 90–111% window is not clinically meaningful when dealing with drugs that have a half-life of 6 hours and a therapeutic window of 2 ng/mL. The fact that this is even debated shows how broken our regulatory system is. There is no bioequivalence when the active ingredient’s crystalline structure differs between manufacturers. This is not science - it’s corporate math.
Anjula Jyala
January 30, 2026 AT 23:05Anyone who switches NTI generics is a walking clinical trial
They’re not patients - they’re data points
Pharmacies don’t care about your INR
Insurance companies care about their quarterly margins
Stop being naive
Stability isn’t a preference - it’s survival
And if you’re on more than one NTI drug? You’re playing Russian roulette with your organs
Kathy McDaniel
January 31, 2026 AT 09:31so i just got my warfarin generic and i think my gums are bleeding more??
not sure if it’s the toothpaste or what
but i’m gonna get my inr checked next week
just wanted to say thanks for this post lol
Paul Taylor
February 1, 2026 AT 02:10Let me tell you something - I’ve been on cyclosporine for 12 years. I started on Sandimmune, then switched to Neoral, then to a generic, then back to Neoral, then to another generic, then back again. I’ve had kidney flares, hypertension spikes, migraines, insomnia - all tied to manufacturer changes. I’ve tracked every single blood level. I’ve talked to every pharmacist in three counties. Here’s what I know: the FDA doesn’t test for inter-generic variability. They test brand vs one generic. But when you switch between Generic A and Generic B - both AB-rated - you’re essentially getting two different drugs. The labels are the same. The pills look the same. But your body knows the difference. And your body doesn’t lie. If you’re stable, don’t touch it. If you’re new, pick one generic and lock it in. Never let the pharmacy swap it. Write DAW 1 on every script. Make your doctor fight for you. Your life isn’t a cost-cutting exercise. It’s a biological masterpiece that deserves consistency.
Desaundrea Morton-Pusey
February 1, 2026 AT 08:31Why are we even talking about this? It’s obvious. Big Pharma owns the FDA. The brand-name companies are scared because generics are cheaper. So they scream ‘danger!’ to scare people into paying $60 a month. Meanwhile, people in Europe and Canada switch NTI generics daily and live perfectly fine. This is pure capitalism disguised as medicine. Stop letting corporations dictate your health.
Murphy Game
February 1, 2026 AT 10:20Did you know the FDA’s NTI registry was created after a whistleblower exposed that two major generic manufacturers altered their dissolution profiles to pass bioequivalence tests? The ‘AB’ rating is a lie. The system is rigged. They don’t test for long-term accumulation. They don’t test for drug interactions. They don’t test what happens when you switch between manufacturers every 3 months. This isn’t about safety - it’s about control. And if you think your pharmacist knows what’s in that pill? You’re the real victim.
John O'Brien
February 1, 2026 AT 13:02Bro I switched my phenytoin to generic and had a seizure in the shower
Woke up in the ER with my wife crying
Turns out the generic had different fillers - slowed absorption
Now I only take Dilantin
Yeah it’s $120 a month
But I’m alive
And I don’t care how much it costs
My brain is worth more
April Williams
February 3, 2026 AT 00:10People like you who say ‘just stay on brand’ are the reason healthcare is so expensive. You’re selfish. You want your $60 pill because you can afford it, but what about the single mom working two jobs who can’t even afford insulin? Stop hoarding safety for yourself. Generics save lives - not just money. If your body can’t handle a $4 pill, maybe you’re not meant to be on the drug at all.
astrid cook
February 4, 2026 AT 08:58You’re all missing the point.
It’s not about brand or generic.
It’s about who controls your prescription.
Insurance companies pick the generic.
Pharmacists don’t ask you.
Doctors don’t fight for you.
And you? You just take what’s handed to you.
That’s the real problem.
Not the pill.
The system.