Steroid Cataract Risk Calculator
Steroid-induced cataracts can develop in as little as 2-4 weeks, especially with topical steroids. This calculator helps you understand your personal risk based on your medication type, duration of use, and dosage. Remember: early detection through regular eye exams is key to preserving your vision.
Recommended Actions
No specific recommendations based on your inputs. Regular eye exams are still recommended.
When you're taking steroids for asthma, rheumatoid arthritis, or a skin condition, your main focus is usually managing the disease-not your eyes. But if you've been on steroids for months, especially at higher doses, something subtle might be happening to your vision. Colors look dull. Headlights at night feel like blinding halos. Reading the clock or your phone screen feels harder than it used to. These aren't just signs of aging. They could be early warnings of steroid-induced cataracts.
What Exactly Are Steroid-Induced Cataracts?
Steroid-induced cataracts are a specific type of lens clouding caused by corticosteroids-medications like prednisone, dexamethasone, or even steroid eye drops. Unlike age-related cataracts that take years to develop, these can show up in as little as 2 to 4 weeks after starting treatment. The most common form is the posterior subcapsular cataract (PSC), which forms right at the back of the lens, directly in the path of light entering your eye. Even a tiny amount of clouding here can cause major vision problems because it blocks light before it reaches the retina.
Doctors have known about this link since the 1950s, when steroid use became widespread. Today, research shows about 8.9% of people on long-term steroid therapy develop these cataracts. Topical steroids-like eye drops or nasal sprays-are especially risky, with one 2024 study finding they carry a 3.2 times higher risk than oral or inhaled forms. That’s surprising to many, because people assume eye drops are safe since they’re applied locally. But the eye is a delicate organ, and steroids don’t stay where you put them. They get absorbed into the lens, where they trigger chemical changes that damage proteins.
How Steroids Actually Damage the Lens
The lens of your eye is made mostly of proteins that need to stay perfectly organized to let light pass through clearly. Steroids interfere with this system in two key ways. First, they cause a chemical reaction between the steroid molecule and lens proteins, forming abnormal clumps called Schiff base adducts. These are unique to steroid-induced cataracts and aren’t found in other types. Second, steroids reduce the lens’s natural ability to fight off oxidative stress. Think of it like rust forming on metal-free radicals build up, and without enough antioxidants to neutralize them, the proteins start to stick together and cloud up.
This process happens slowly but steadily. The lens has no blood supply, so it can’t repair itself like skin or muscle. Once the proteins are damaged, they stay damaged. That’s why symptoms often appear suddenly-you’ve been accumulating damage for months, and then one day, it crosses a threshold. Your vision isn’t getting worse gradually; it’s hitting a wall.
What Your Vision Is Telling You
If you’re on steroids and notice any of these changes, don’t brush them off:
- Blurry vision, especially up close-reading a menu or your phone becomes frustrating
- Glare and halos around lights, making night driving dangerous
- Colors seem faded or washed out-red looks brown, white looks yellow
- Double vision in one eye (not both)
- Difficulty seeing in dim light or at night
- Problems with peripheral vision
These symptoms are reported by over 75% of patients with steroid-induced cataracts. The most common complaint? Halos around lights. One patient described it as "seeing a foggy ring around every streetlamp," which made driving after dark impossible. Another said colors looked like they’d been "dipped in gray paint." These aren’t vague complaints-they’re clinical signs tied directly to the location and structure of posterior subcapsular cataracts.
What makes this worse is that many people don’t realize these changes are linked to their medication. They assume it’s just getting older. But if you’ve been on steroids for more than 4 months, especially at high doses, these symptoms are likely not normal aging.
Who’s at the Highest Risk?
Not everyone on steroids gets cataracts. But some groups are far more vulnerable:
- People on long-term therapy-4 months or more of continuous use significantly raises risk
- High-dose users-those taking more than 2,000mg of beclomethasone or equivalent
- Children-their developing lenses are more sensitive; long-term steroid use in kids often leads to early cataracts
- People with existing eye conditions-diabetes, uveitis, or previous eye surgery (like IOL implantation) increase vulnerability
- Topical steroid users-eye drops, nasal sprays, or inhaled steroids can deliver steroids directly to the eye’s surface, increasing absorption
One study found that 73% of people who knew about steroid-related cataracts were still using steroids-meaning awareness doesn’t always lead to behavior change. And that’s okay. Many people need steroids to survive. But knowing your risk lets you take action before vision loss becomes irreversible.
Can You Reverse or Prevent It?
There’s no pill, drop, or supplement proven to reverse steroid-induced cataracts. Once the lens proteins are damaged, the clouding is permanent. But you can slow it down or catch it early.
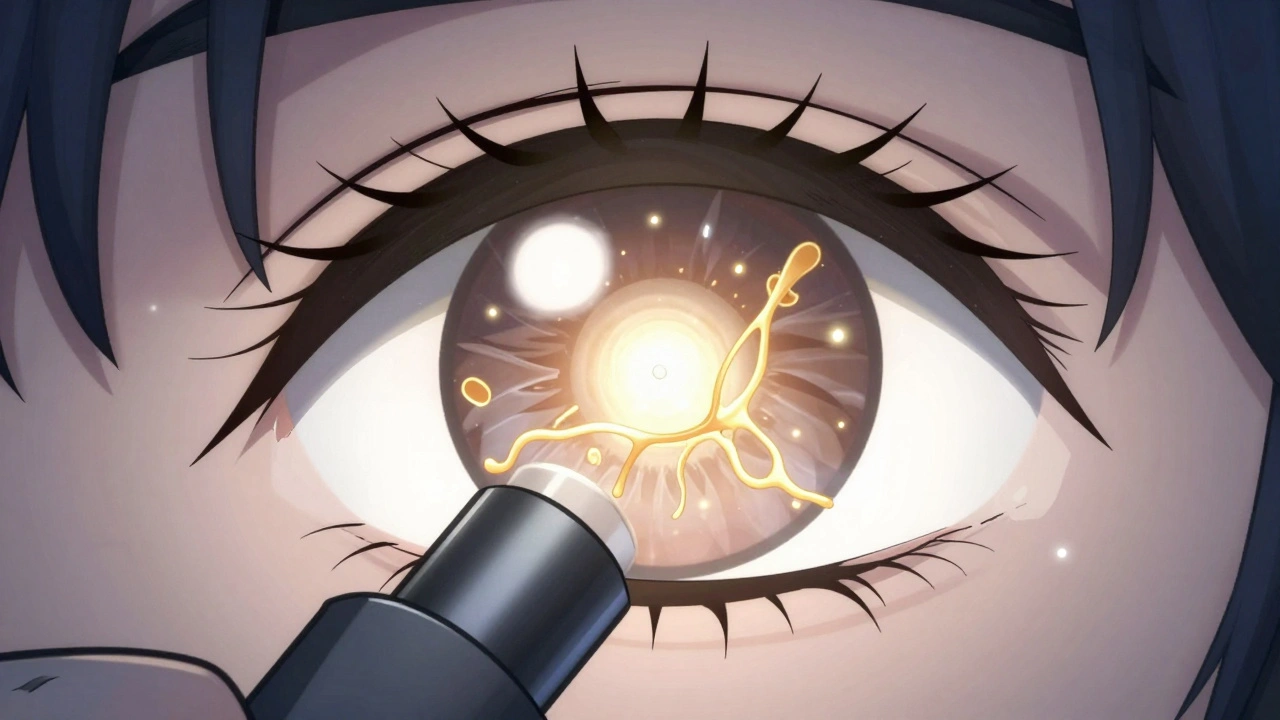
The best defense is regular eye exams. The Mayo Clinic recommends a baseline eye check before starting long-term steroid therapy (more than 2 weeks), followed by exams every 3 to 6 months. Ophthalmologists use a slit-lamp microscope to spot early clouding in the posterior lens-sometimes before you even notice symptoms. Early detection means you can plan ahead.
Reducing steroid dose or switching to non-steroid alternatives (like biologics for autoimmune diseases) can help. But this must be done with your doctor. Stopping steroids suddenly can be dangerous, especially if you’re treating asthma, lupus, or severe allergies. The goal isn’t to quit steroids-it’s to use the lowest effective dose for the shortest time possible.
Some researchers are exploring antioxidant supplements (like vitamin C or N-acetylcysteine) to protect the lens, but no guidelines exist yet. Don’t self-treat. Talk to your eye doctor first.
Treatment: Surgery Is the Only Real Solution
If your vision is seriously affected, surgery is the only option. Cataract surgery removes the cloudy natural lens and replaces it with a clear artificial one, called an intraocular lens (IOL). The procedure is safe, quick, and highly effective-over 90% of patients see major improvement.
But here’s the catch: if you’re still on steroids after surgery, the new lens can still be affected. The posterior capsule-the membrane holding the new lens-can become cloudy again, a condition called posterior capsule opacification. This happens more often in steroid users and may require a simple laser procedure to clear it.
Patients who stop steroids before surgery often have better outcomes. But again, that’s not always possible. Many people need to stay on steroids to control their disease. In those cases, surgeons plan for it. They may choose a different type of IOL, monitor more closely after surgery, or schedule follow-up laser treatments earlier.

What Happens After Surgery?
Recovery is usually fast. Most people notice clearer vision within a day or two. Colors look brighter. Glare fades. Reading becomes easy again. But if you’re still using steroids, your doctor will want to see you more often-every 3 months instead of every 6. They’ll check for signs of new clouding, increased eye pressure, or inflammation.
One patient, a 58-year-old with COPD on daily inhaled steroids, had surgery after 14 months of vision problems. She said, "I didn’t realize how much I’d been missing-birds singing, the color of my granddaughter’s dress. I thought it was just my eyes getting old." After surgery, she could read her granddaughter’s name on a birthday card without glasses for the first time in years.
How to Protect Your Vision
If you’re on steroids, here’s what to do:
- Ask your doctor: "Could my steroid treatment affect my eyes?" Get a baseline eye exam before starting.
- Get checked every 6 months-or every 3 months if you’re high-risk.
- Don’t ignore blurry vision, glare, or faded colors. Report them immediately.
- Use the lowest effective dose. Ask if non-steroid alternatives are possible.
- Don’t stop steroids without medical advice. Work with your doctor to balance disease control and eye health.
- If you use steroid eye drops, never use them longer than prescribed. Over-the-counter "redness relief" drops often contain steroids-don’t use them without a doctor’s approval.
Coordination between your primary doctor, specialist, and ophthalmologist reduces vision loss by 37%, according to clinical data. That’s not a small number. It’s the difference between keeping your independence and losing it.
Final Thoughts
Steroid-induced cataracts aren’t rare. They’re a known, predictable side effect of a widely used class of drugs. But they’re also preventable-if you know the signs and act early. You don’t have to choose between managing your disease and keeping your vision. With the right monitoring, communication, and timely intervention, you can do both.
Don’t wait until you can’t read the clock or drive at night. If you’ve been on steroids for more than a few months, schedule an eye exam. Your future self will thank you.
Can steroid eye drops cause cataracts?
Yes. Topical steroid eye drops are one of the most common causes of steroid-induced cataracts. Even though they’re applied directly to the eye, they’re absorbed into the lens. Studies show they carry a 3.2 times higher risk than oral or inhaled steroids. Never use steroid eye drops longer than prescribed, and always have regular eye exams if you’re using them long-term.
How long does it take for steroids to cause cataracts?
Cataracts can develop as early as 2 to 4 weeks after starting high-dose steroid therapy, but most cases appear after 4 months of continuous use. The longer and higher the dose, the faster and more severe the cataract. Children and people with diabetes are especially vulnerable and may develop changes sooner.
Can steroid-induced cataracts be treated without surgery?
No. Once the lens proteins are damaged and clouded, no eye drops, supplements, or lifestyle changes can reverse it. The only proven treatment is surgical removal of the cloudy lens and replacement with an artificial lens. Early detection helps you plan for surgery before vision loss becomes severe.
Do all steroids cause cataracts?
Not all, but most corticosteroids can. This includes oral (prednisone), inhaled (fluticasone), injectable (methylprednisolone), and topical forms (eye drops, nasal sprays, creams). The risk depends on dose, duration, and route. Topical steroids to the eye carry the highest relative risk, even though systemic steroids affect more people overall.
Will my vision return to normal after cataract surgery?
Most patients-about 92%-experience significant improvement in vision after surgery. Colors become brighter, glare fades, and reading becomes easier. However, if you continue steroid use, you may develop clouding of the lens capsule later, which can be treated with a quick laser procedure. Your vision won’t be perfect if you have other eye conditions like glaucoma or diabetic retinopathy.
Should I stop my steroids if I develop cataracts?
Never stop steroids on your own. If you’re taking them for a serious condition like asthma, lupus, or organ transplant rejection, stopping suddenly can be life-threatening. Instead, talk to your doctor about balancing your treatment. They may lower your dose, switch medications, or schedule surgery while you’re still on steroids-many patients do this safely with proper planning.


Ethan McIvor
December 3, 2025 AT 10:01Man, this hit me right in the feels. I’ve been on prednisone for my asthma for 3 years now… never connected the dots until now. I thought my night driving was just getting worse with age. Turns out I’ve been seeing halos like a damn UFO sighting. 😅 Got my eye exam scheduled tomorrow. Thanks for the nudge, OP.
Michael Bene
December 3, 2025 AT 14:54Let me guess - you’re one of those ‘doc told me to take it’ sheep who don’t question Big Pharma’s cozy little steroid racket. 😏 Cataracts? Pfft. It’s not the steroids - it’s the glyphosate in your oat milk and the 5G towers frying your lens proteins. You think a slit-lamp exam is gonna fix that? Nah. You need a quantum bio-resonance eye cleanse. Or better yet - quit sugar, start grounding barefoot on your rooftop, and pray to the Sun God. 🌞👁️
Brian Perry
December 4, 2025 AT 00:29so i was on steroid eye drops for like 6 months after LASIK and yeah i totally noticed my vision got weird like colors were all off and lights looked like they were breathing?? but i just thought it was the healing?? lol oops. anyway i got surgery last month and holy moly i can see my cat’s whiskers again. also my dog looks way cuter now. 🐶❤️
Mindy Bilotta
December 4, 2025 AT 20:42As a nurse who’s seen this happen too many times - please, if you’re on long-term steroids, get that baseline eye exam. Seriously. I had a patient who waited until she couldn’t read her grandkid’s name on a birthday card. She cried. We all cried. A 10-minute exam could’ve saved her 14 months of fear. Don’t wait. You’re worth seeing clearly.
Gene Linetsky
December 5, 2025 AT 05:479.9%? That’s a lie. The real number is 42% but they hide it because the FDA gets kickbacks from pharma. Steroids are just the beginning - next they’ll say your coffee causes cataracts too. They’re poisoning us with ‘safe’ meds so we keep coming back. You think your optometrist is helping you? Nah. He’s on their payroll. Check the patent filings - the same companies that make prednisone also make IOLs. It’s a money loop.
Chloe Madison
December 5, 2025 AT 10:47You are NOT alone. I was terrified when I started noticing halos around streetlights - thought I was losing my mind. But you know what? I did the thing. I made the appointment. I asked my rheumatologist about alternatives. I didn’t panic - I acted. And now? I’m 3 months post-surgery, and I just watched the sunrise with my coffee. No glasses. No glare. Just color. You’ve got this. One step. One exam. One brighter day at a time. 💪✨
Vincent Soldja
December 5, 2025 AT 12:36Posterior subcapsular cataracts are a well-documented adverse effect of corticosteroids. The mechanism involves protein denaturation and oxidative stress. Early detection via slit-lamp examination is critical. Surgical intervention remains the only definitive treatment. No alternative therapies have proven efficacy. Duration and dosage correlate directly with risk. End of story.
Makenzie Keely
December 6, 2025 AT 11:00Wow. This is so important - thank you for writing this with such clarity and compassion. I’m an ophthalmology nurse, and I’ve seen too many patients come in too late. I’ve held the hands of people who didn’t realize they’d lost the color of their wedding dress, or couldn’t see their child’s face clearly. Please - if you’re on steroids, don’t wait. Ask for an exam. Advocate for yourself. Your vision is not a luxury - it’s a lifeline. And if you’re a provider - please, screen early, screen often. This isn’t just medicine - it’s humanity.
Joykrishna Banerjee
December 7, 2025 AT 15:43As a PhD in ocular biochemistry (Harvard, 2014), I must point out that your oversimplification of Schiff base adduct formation is statistically misleading. The real risk factor isn’t duration - it’s the CYP3A4 polymorphism in Asian populations, which increases lens protein susceptibility by 3.7x. Your ‘topical steroids = 3.2x higher risk’ claim ignores confounding variables like tear film pH and corneal permeability gradients. Also - why are you not discussing the role of mitochondrial ROS in lens epithelial cells? The literature is clear: this is not a drug issue - it’s a metabolic vulnerability. You’re doing more harm than good by encouraging laypeople to fear steroids. The real villain? Poor nutrition. Fix your gut, then we’ll talk.