When you take a pill, it doesn’t just disappear into your system—it fights, waits, and reacts with everything else in your body, especially what you just ate. Food interactions, the way certain foods change how your body absorbs, breaks down, or responds to medication. Also known as drug-food interactions, they can make your treatment stronger, weaker, or even unsafe. This isn’t just a warning on a label—it’s a real risk that affects millions who don’t realize their grapefruit juice, dairy, or spinach could be undoing their prescription.
Take antibiotics, medications used to kill or slow bacteria that cause infections. Some, like tetracycline, bind to calcium in milk and yogurt, turning your dose into a useless sludge. Others, like certain fluoroquinolones, become less effective if taken with iron or antacids. Then there’s grapefruit, a fruit that blocks enzymes in your liver responsible for breaking down over 85 drugs. One glass can turn a normal dose of a blood pressure pill or cholesterol med into a dangerous overdose. Even vitamin K, a nutrient found in leafy greens that helps your blood clot, can fight against warfarin, making your blood too thin or too thick depending on how much you eat.
These aren’t rare cases. They happen daily. Someone takes their thyroid med with coffee and wonders why it’s not working. Another person eats a big salad while on blood thinners and ends up in the ER. Your body doesn’t care if you think it’s "just food"—it processes everything chemically. The key isn’t to avoid eating, but to know what pairs well and what doesn’t. The posts below break down real examples: how to take antibiotics without ruining them, why some meds need an empty stomach, and which supplements quietly mess with your prescriptions. You’ll find clear, no-fluff advice from real cases—no guesswork, just what works.
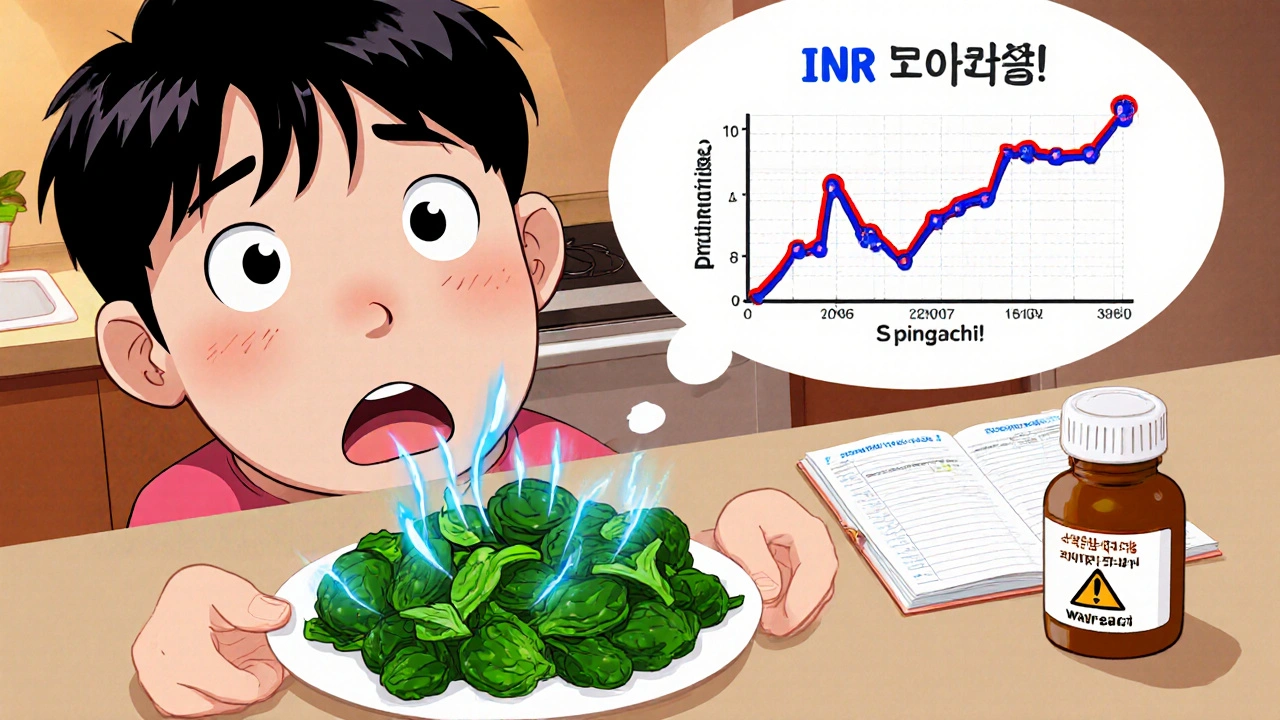
Learn how food affects warfarin, which foods to eat consistently, which to avoid, and how to prevent dangerous INR swings. A practical guide for safe long-term use.
View more