When talking about HSDD, Hypoactive Sexual Desire Disorder is a persistent lack of sexual interest that causes distress or relationship problems. Also known as low sexual desire, it affects both men and women and often goes unnoticed until it interferes with daily life. HSDD isn’t just a mood swing; it’s a medical condition that can be linked to hormones, mental health, and lifestyle factors. This paragraph sets the stage for the deeper dive that follows.
One of the most common companions of HSDD is Erectile Dysfunction, the inability to achieve or maintain an erection sufficient for sexual activity. While ED is often discussed in men, the two conditions share underlying mechanisms such as vascular health and hormone balance. When ED is present, it can amplify the frustration of low desire, creating a feedback loop that worsens both problems.
Another key player is Hormone Replacement Therapy, the use of estrogen, testosterone, or other hormones to correct deficiencies that affect sexual function. Hormonal shifts during menopause, androgen decline in men, or thyroid irregularities can trigger HSDD. Addressing these imbalances with targeted therapy often restores desire more quickly than psychotherapy alone.
Psychological support comes in the form of Sex Therapy, a counseling approach focused on improving sexual communication, desire, and satisfaction. Sex therapists use techniques like sensate focus, guided mindfulness, and couple exercises to rekindle interest. Research shows that when sex therapy is combined with medical treatment, patients report higher satisfaction and lower relapse rates.
Beyond these three, mental health conditions such as anxiety, depression, and past trauma also shape desire. The brain’s reward pathways can become desensitized, making ordinary intimacy feel unfamiliar. Addressing stressors, sleep quality, and nutrition rounds out a holistic plan for HSDD.
Diagnosis starts with a detailed history and validated questionnaires like the Decreased Sexual Desire Screener. Doctors rule out medical causes—thyroid disorders, diabetes, medication side effects—before labeling the problem as HSDD. This systematic approach ensures that treatment targets the right root cause.
When it comes to medication, options like flibanserin for women and bupropion for men act on neurotransmitters to boost desire. These drugs are most effective when paired with lifestyle tweaks—regular exercise, balanced diet, and reduced alcohol intake—which naturally enhance hormone levels and mood.
For couples, communication is the linchpin. Open conversations about fantasies, boundaries, and expectations create a safe space where desire can flourish. Joint counseling sessions can help partners navigate mismatched libidos without blame.
Therapeutic plans often follow a three‑step model: identify biological contributors, address psychological barriers, and reinforce positive sexual experiences. This model illustrates the semantic triple that HSDD encompasses low desire, requires hormone therapy, and benefits from sex therapy. Each step builds on the previous, creating a comprehensive roadmap.
Finally, tracking progress with simple tools—monthly desire scales, mood journals, or digital apps—helps patients and clinicians adjust treatment in real time. Regular follow‑ups ensure that any side effects or new stressors are caught early, keeping the recovery trajectory upward.
Below you’ll find a curated list of articles that dive deeper into the specific treatments, lifestyle tips, and scientific insights mentioned here. Whether you’re looking for medication comparisons, therapy techniques, or hormone guidance, the collection offers practical takeaways you can apply right away.
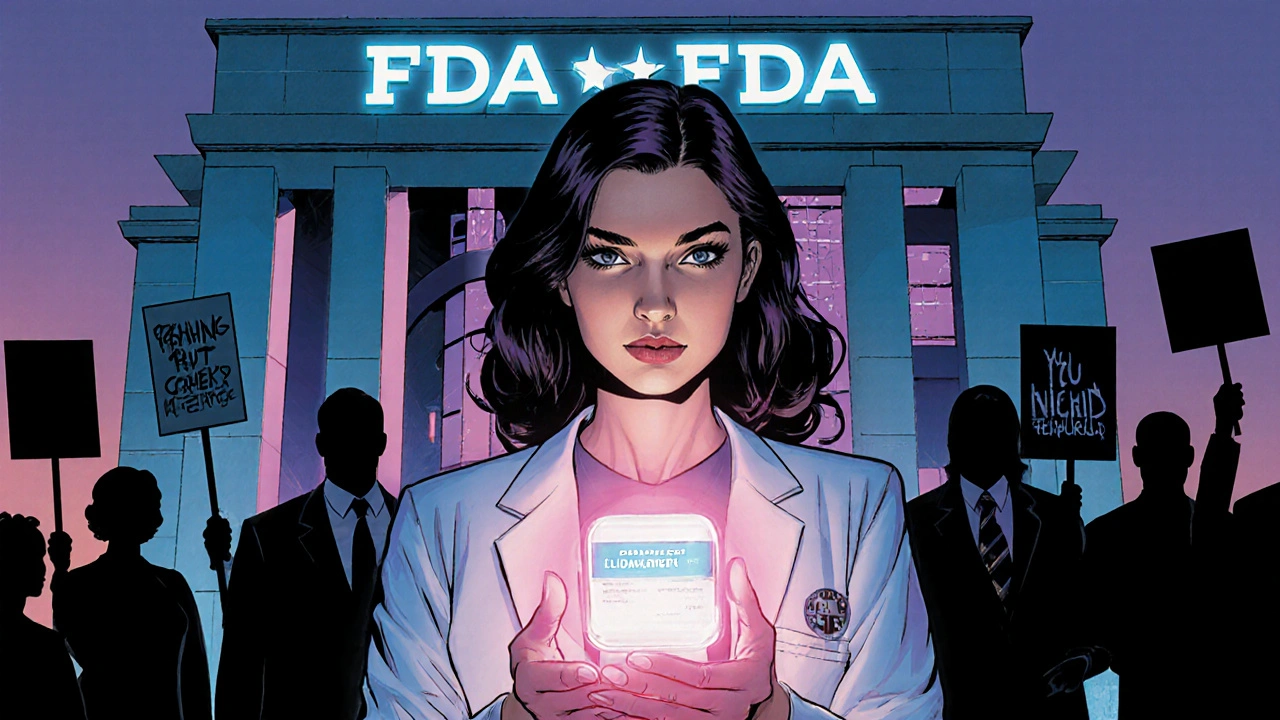
Explore flibanserin's role in treating low sexual desire, its controversial FDA approval, safety profile, gender bias in research, and the ongoing fight for female sexual equality.
View more