When we talk about antibiotic stewardship, the practice of using antibiotics only when needed and in the right way to protect their effectiveness. Also known as antimicrobial stewardship, it’s not just a hospital policy—it’s something that affects every person who’s ever taken a pill for a sore throat or a sinus infection. Too many people think antibiotics cure everything: colds, flu, even mild earaches. But antibiotics don’t work on viruses. When they’re used too often or the wrong way, bacteria learn to fight back—and that’s how antibiotic resistance, when bacteria evolve to survive drug exposure becomes a global crisis. The World Health Organization calls it one of the top 10 public health threats we face. And it’s not some distant future problem—it’s happening right now, in clinics, homes, and pharmacies.
Antibiotic stewardship isn’t about avoiding antibiotics altogether. It’s about using them like a scalpel, not a hammer. That means: only prescribing them when there’s clear bacterial evidence, choosing the narrowest-spectrum drug possible, giving the right dose for the right length of time, and never saving leftover pills for next time. Hospitals use teams of pharmacists and doctors to monitor prescriptions. But you don’t need a medical degree to be part of the solution. If your doctor says you don’t need an antibiotic, trust them. If you’re given one, finish the full course—even if you feel better. Skipping doses or stopping early is one of the biggest reasons resistant strains survive and spread.
There’s a direct link between what’s in your medicine cabinet and what ends up in the environment. When antibiotics are overused, traces show up in water, soil, and even food. That’s why appropriate antibiotic use, the core principle of stewardship that balances treatment needs with long-term safety matters beyond your body. It’s about protecting future generations from untreatable infections. And it’s not just about prescriptions. The same logic applies to livestock farming, where antibiotics are often used to speed up growth—not to treat illness. That’s why some countries have banned non-therapeutic use, and why you should care about where your meat comes from.
What you’ll find in these posts isn’t just a list of drugs. It’s a look at real alternatives—like how azithromycin compares to doxycycline, or why Tamiflu isn’t an antibiotic but still gets confused with one. You’ll see how people are using topical treatments, herbal supports, and smarter diagnostics to reduce unnecessary antibiotic pressure. These aren’t theoretical debates. These are choices real patients and doctors are making every day to keep antibiotics alive. This collection shows you how to spot when a drug is truly needed—and when it’s just noise. No fluff. No fearmongering. Just clear, practical info to help you make smarter calls with your health.
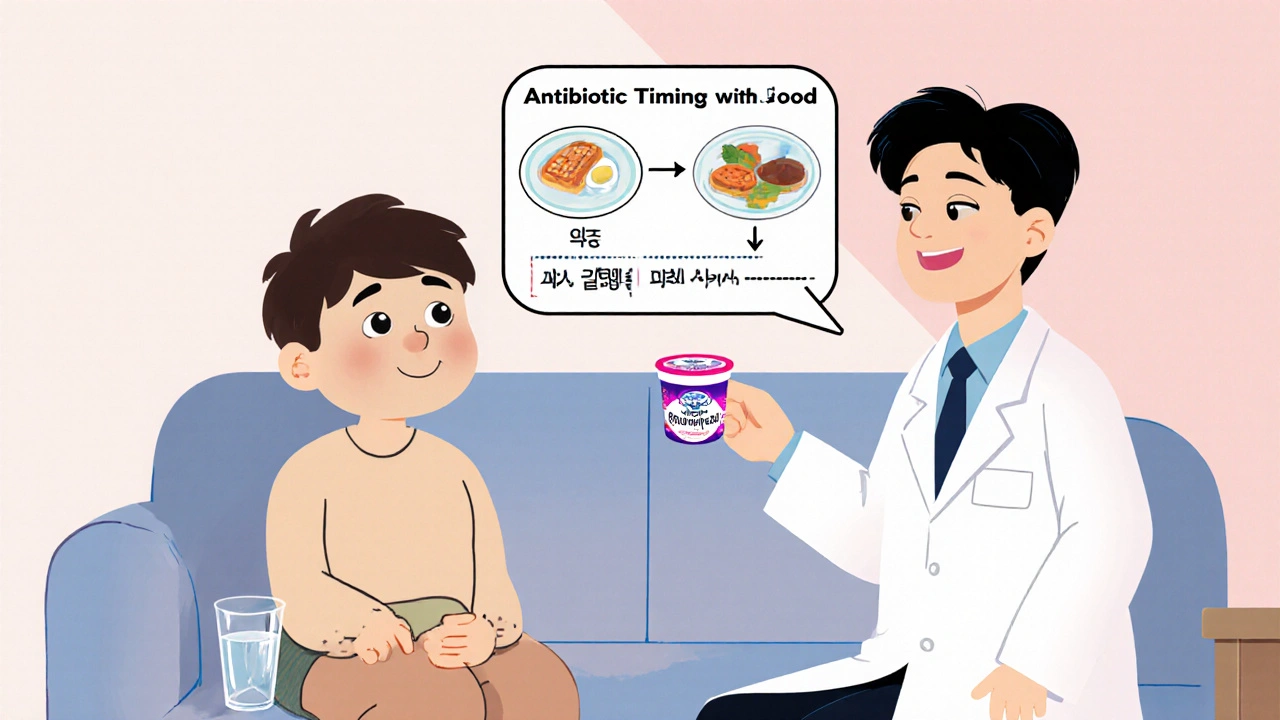
Learn how to manage common antibiotic side effects like nausea, diarrhea, and sun sensitivity without stopping your course. Practical tips backed by medical guidelines to help you finish your prescription safely.
View more