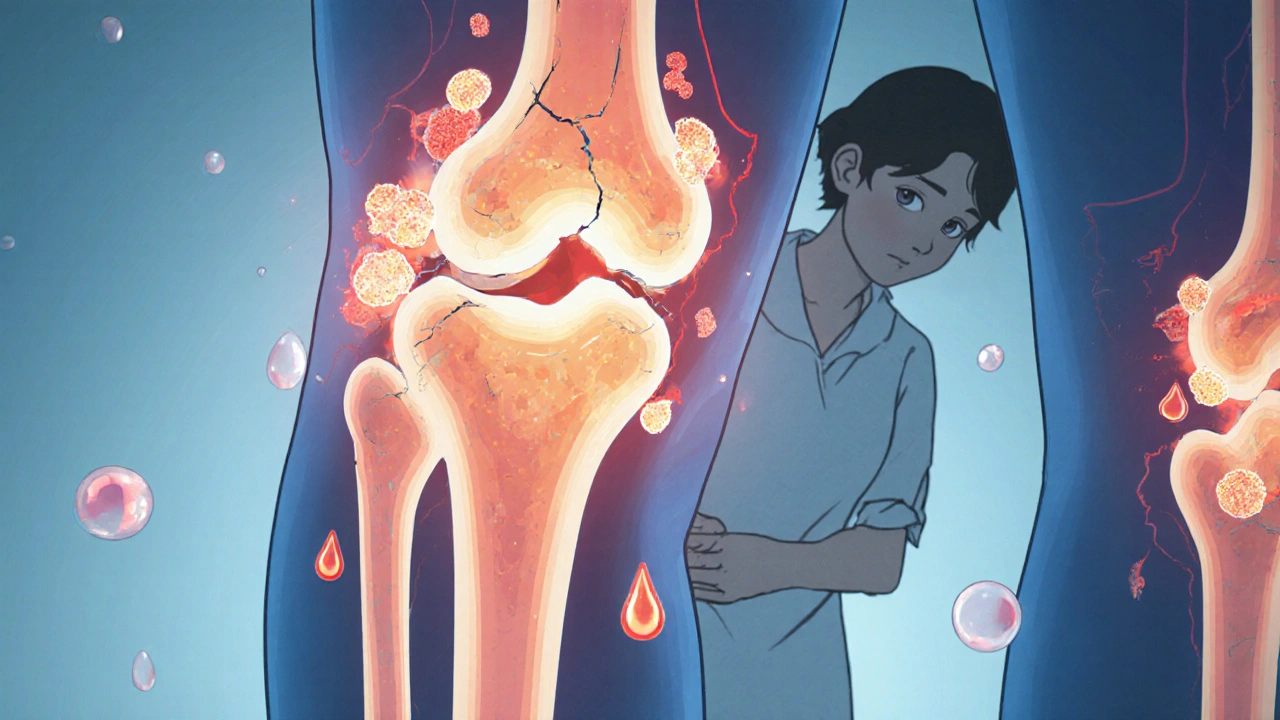
When dealing with bisphosphate therapy, a class of drugs that slow bone loss by inhibiting osteoclast activity. Also known as bisphosphonates, it is a cornerstone in managing conditions like osteoporosis. This approach targets the cells that break down bone, giving the skeleton a chance to rebuild stronger.
It primarily addresses osteoporosis, a disease marked by reduced bone mineral density and increased fracture risk. People with low bone mineral density (BMD) often see rapid bone loss after menopause or with long‑term steroid use. By curbing the bone‑resorbing process, bisphosphate therapy helps raise BMD scores and lowers the chance of hip or vertebral fractures.
Two main delivery routes exist: oral pills and intravenous administration, a infusion given in a clinic that bypasses the gut. Oral forms (like alendronate) require fasting and upright posture to avoid esophageal irritation, while IV drugs (such as zoledronic acid) deliver the full dose in minutes and skip GI side effects. The choice often depends on patient convenience, kidney function, and how quickly a clinician wants to see a BMD boost.
Dosage schedules vary widely. Some patients take a weekly tablet, others a monthly dose, and a few receive an annual infusion. The less‑frequent the dosing, the easier it is to stay adherent—adherence is a key predictor of treatment success. Studies show that patients who miss fewer than 20% of doses see a measurable rise in bone density within a year.
Every medication has downsides, and bisphosphate therapy is no exception. adverse effects, include gastrointestinal upset, acute phase reactions, and rare osteonecrosis of the jaw can hinder long‑term use. GI irritation is most common with oral pills, while flu‑like symptoms often follow IV infusions. Early detection of side effects and proper dental care before starting therapy can dramatically lower the risk of severe complications.
Monitoring is essential. Doctors usually order a dual‑energy X‑ray absorptiometry (DXA) scan at baseline and then every 1–2 years to track bone mineral density changes. Lab tests for calcium, vitamin D, and kidney function are also routine, because low vitamin D or impaired renal clearance can worsen side effects. Adjusting the dose or switching delivery routes based on these results keeps the treatment both safe and effective.
Beyond bone health, bisphosphate therapy can impact other systems. Some research links long‑term use to atypical femoral fractures, especially in patients who have been on the drugs for over five years. A “drug holiday” after several years of continuous therapy is often recommended to balance benefits against these rare risks. Discussing the timing of a holiday with a healthcare provider ensures the bone remains protected while minimizing harm.
All of these points—how the drugs work, the conditions they treat, the delivery methods, dosing schedules, side‑effect management, and monitoring—form the backbone of effective bisphosphate therapy. bisphosphate therapy offers a powerful way to strengthen fragile skeletons, but it works best when patients, clinicians, and pharmacies coordinate the right drug, dose, and follow‑up plan. Below you’ll find a curated set of articles that dive deeper into specific drugs, comparisons, safety tips, and real‑world experiences, giving you a complete picture of what to expect and how to get the most out of your treatment.
Explore how alendronate helps cancer patients with bone metastases, its benefits, safety, and when to choose it over IV options.
View more