When someone is diagnosed with HER2-positive breast cancer, a subtype of breast cancer driven by excess HER2 protein that makes cancer cells grow faster. Also known as HER2+ breast cancer, it accounts for about 15–20% of all breast cancer cases and used to be one of the most aggressive forms—until targeted treatments changed the game. This isn’t just another type of breast cancer. It’s defined by a specific biological marker: too much HER2 protein on the surface of cancer cells. That overexpression doesn’t just make the cancer grow faster—it also gives doctors a clear target for treatment.
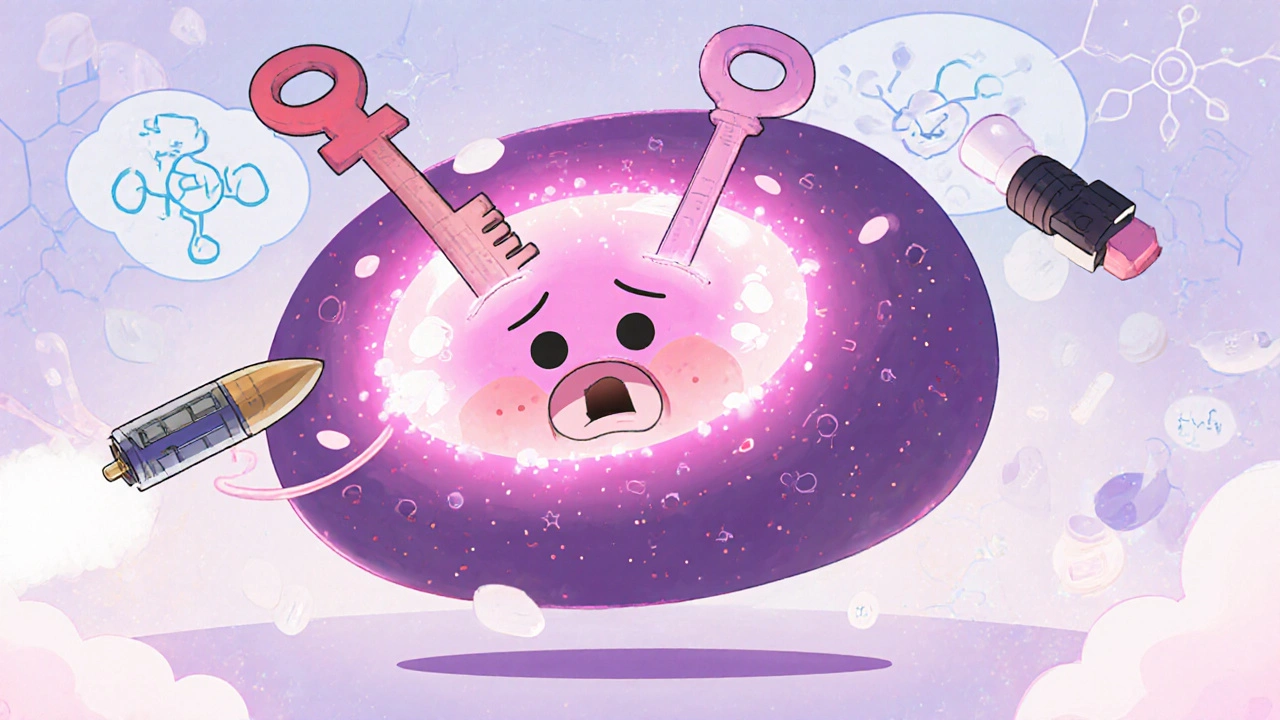
Testing for HER2 status is standard after a breast cancer diagnosis. Pathologists use either IHC (immunohistochemistry) or FISH (fluorescence in situ hybridization) to check how much HER2 is present. If it’s positive, the treatment path shifts dramatically. Instead of relying only on chemo or hormones, doctors add trastuzumab, a monoclonal antibody that locks onto HER2 proteins and blocks cancer growth. Also known as Herceptin, it was one of the first precision cancer drugs to show real survival benefits. Trastuzumab doesn’t work alone. It’s often paired with chemo, and sometimes with other HER2 blockers like pertuzumab or ado-trastuzumab emtansine (T-DM1). These combinations have turned what was once a poor prognosis into a manageable, even curable, condition for many.
But HER2-positive breast cancer isn’t one-size-fits-all. Some patients respond for years. Others see the cancer come back. That’s why newer drugs like tucatinib and fam-trastuzumab deruxtecan are now in use—especially for advanced cases. And while targeted therapies are powerful, they still come with side effects: heart issues, diarrhea, fatigue. Monitoring is part of the treatment. Patients need regular echocardiograms, blood tests, and open conversations with their oncology team.
The good news? Survival rates for HER2-positive breast cancer have jumped dramatically over the last 20 years. Early-stage patients now have survival rates close to 90% with the right treatment plan. Even in later stages, many people live for years with good quality of life. What matters most is getting tested correctly, starting treatment early, and sticking with the plan. It’s not about hoping for the best—it’s about using the science that’s already here.
Below, you’ll find real-world guides on managing side effects, comparing treatments, understanding drug interactions, and navigating life with this diagnosis. From how to handle nausea from chemo to knowing when generic versions are safe, these posts give you the details you won’t get in a one-minute doctor’s visit.
HER2-positive breast cancer, once aggressive and hard to treat, now has multiple targeted therapies that improve survival and quality of life. Learn how trastuzumab, T-DXd, tucatinib, and other drugs work, their side effects, and what’s next in treatment.
View more