When you take a pill, you expect it to help—not hurt. But medication errors, mistakes in prescribing, dispensing, or taking drugs that lead to harm. Also known as drug errors, they’re one of the most common causes of preventable hospital visits in the U.S. These aren’t just typos on a label. They’re a 10-year-old getting an adult dose, an elderly patient mixing two drugs that clash, or a pharmacy giving the wrong pill because the labels look too similar. And they happen more often than you think—studies show over 1.5 million people are injured every year in the U.S. alone because of them.
Dosing mistakes, incorrect amounts of medication given or taken. Also known as miscalculated doses, it’s one of the biggest risks for kids and seniors. Pediatric dosing is especially tricky—getting the mg/kg calculation wrong by a decimal point can be deadly. That’s why weight-based calculations and double-checking with a pharmacist aren’t optional. For older adults, it’s not just about the dose—it’s about stacking five different prescriptions without realizing they interact. Drug interactions, harmful effects when two or more medications are taken together. Also known as medication conflicts, they’re behind many ER trips, especially with blood thinners, opioids, and antidepressants. Warfarin and leafy greens, opioids and anti-nausea drugs, SSRIs and migraine meds—these combos can turn a routine treatment into a crisis.
Pharmacy errors, mistakes made when filling prescriptions. Also known as dispensing errors, they’re often hidden in plain sight. A bottle labeled "Lipitor" but filled with a generic statin? Fine—unless you’re allergic to the filler. A label that says "take once daily" but the script meant twice? That’s how people end up with toxic levels. And it’s not just about the pill. Prescription safety, the system of checks and clear communication that keeps drugs from being misused. Also known as medication safety, it includes everything from electronic prescribing to large-print labels for low-vision users. If you can’t read your label, you can’t take your medicine right. That’s why pharmacies now offer ScripTalk and audio labels—but you have to ask for them.
These aren’t abstract risks. They’re everyday dangers. A parent giving the wrong dose of Tylenol. A grandparent mixing painkillers with sleep aids. A patient switching generics without knowing the fillers changed. The system isn’t perfect. But you don’t have to be passive. You can ask questions. You can check labels. You can bring a list of everything you take to every appointment. The posts below show you exactly how—whether it’s how EHR systems are cutting errors in 2025, why pediatric dosing needs a second look, or how accessible labels prevent disasters. You’re not just reading about medication errors. You’re learning how to stop them before they happen.
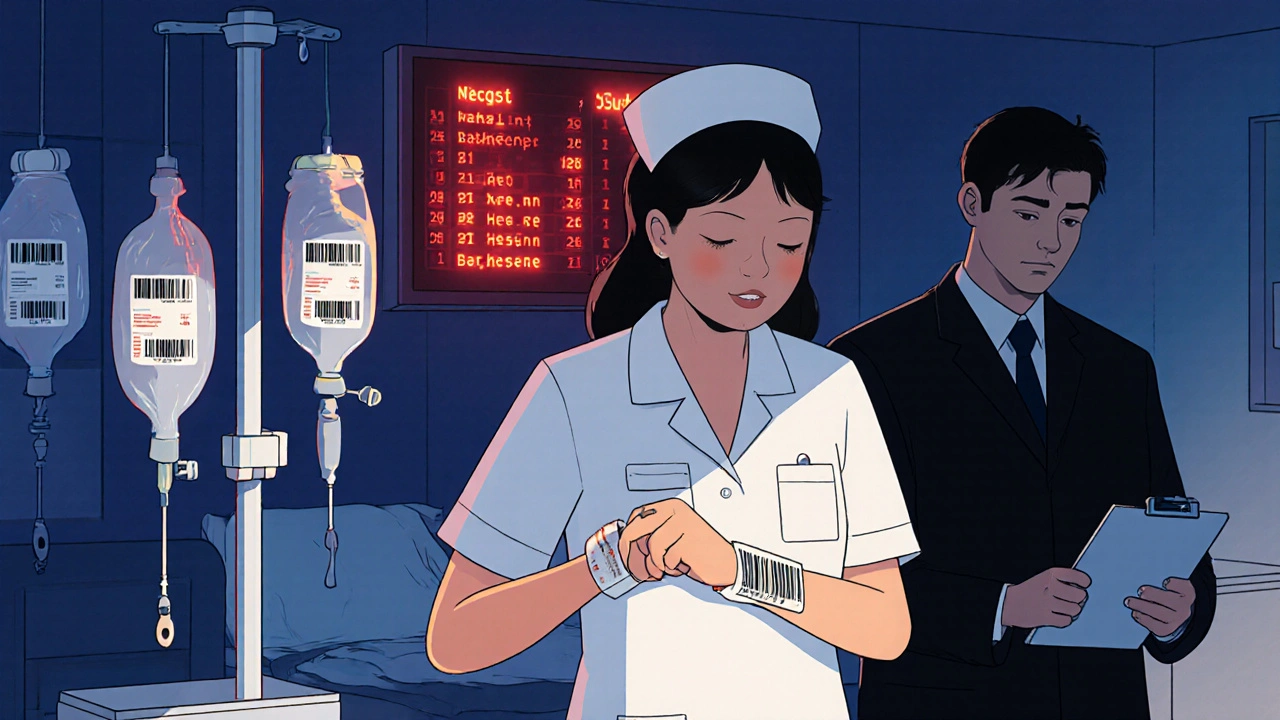
Medication errors are common in both hospitals and retail pharmacies, but the types, causes, and consequences differ. Learn how errors happen in each setting and what you can do to protect yourself.
View more