When a doctor writes a prescription, it’s supposed to be the start of healing—not the beginning of a dangerous mistake. Prescription errors, mistakes in writing, filling, or taking a medication that can lead to harm or death. Also known as medication errors, they’re one of the most common causes of preventable hospital injuries in the U.S. These aren’t just typos. They’re wrong doses, confused drug names, ignored allergies, or pills meant for a child given to an adult. And they happen more often than you think.
Electronic prescribing, the digital transmission of prescriptions from doctor to pharmacy was meant to cut these errors down. And it has—by a lot. But it’s not perfect. Pharmacies still get confused when systems don’t talk to each other. A patient might get a drug that clashes with another they’re already taking because their allergy history didn’t transfer. Or a nurse misreads a digital dose because the screen is too small. Pharmacy communication, how providers and pharmacists share patient data and clarify orders is still broken in too many places. Even small delays or missing details can cost someone their health.
Some errors happen at home. A parent gives a child the wrong amount because they didn’t convert milligrams to milliliters right. An older adult mixes up pills because the label is too small. A person on warfarin eats spinach one day and skips it the next, throwing off their blood thinning. Dosing mistakes, incorrect amounts of medication given or taken are especially deadly in kids and seniors. Weight-based calculations for children? A single decimal error can be fatal. And for seniors on five or more meds? One wrong pill can send them to the ER.
It’s not all bad news. Pharmacies now offer large print labels for people with low vision. Some systems flag dangerous combinations before the pill even leaves the counter. Doctors are learning to double-check high-risk drugs like insulin and opioids. And patients are starting to ask more questions—because they should. If a pill looks different than last time, ask why. If the dose seems too high or too low, question it. You’re not being difficult—you’re protecting yourself.
This collection of articles dives into the real-world causes of these mistakes and how people are fighting back. You’ll find guides on how to calculate safe doses for children, why generic drugs sometimes cause confusion, how EHR systems can either help or hurt, and what to do if you suspect a pharmacy made a mistake. You’ll also see how simple fixes—like better labels, clearer communication, and patient education—are saving lives every day. These aren’t theoretical ideas. They’re real solutions being used right now. And they’re the reason fewer people are getting hurt by something that was meant to help them.
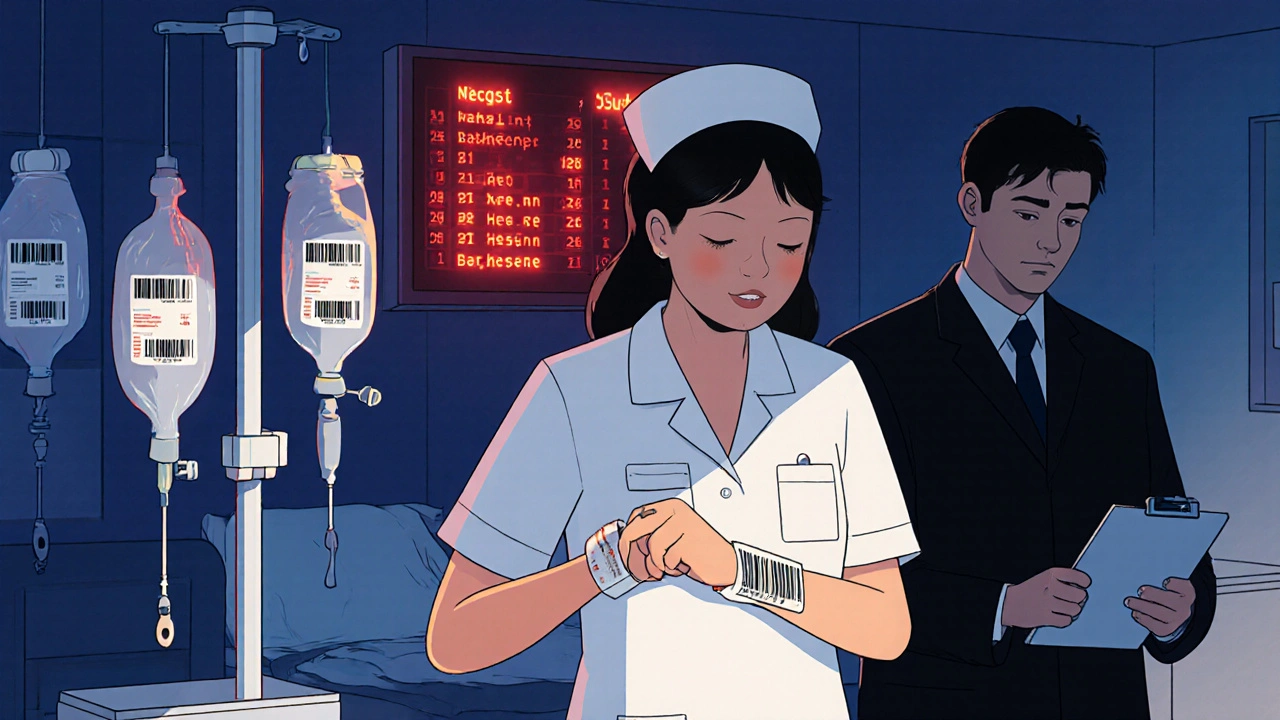
Medication errors are common in both hospitals and retail pharmacies, but the types, causes, and consequences differ. Learn how errors happen in each setting and what you can do to protect yourself.
View more