When you walk into a retail pharmacy, a local drugstore where prescriptions are filled and over-the-counter medicines are sold. Also known as community pharmacy, it's meant to be a safe place for your health—but mistakes happen more often than you think. A wrong dose, a mislabeled bottle, or a missed drug interaction can turn a simple visit into a crisis. These aren’t rare glitches. Studies show that retail pharmacy mistakes contribute to over 1.3 million patient injuries in the U.S. every year. Most aren’t from laziness or malice. They’re from rushed workflows, poor communication, and systems that don’t catch simple human errors.
One of the biggest issues is prescription accuracy, how correctly a pharmacist reads, interprets, and fills a doctor’s order. Handwritten scripts, similar drug names like hydroxyzine and hydralazine, or unclear abbreviations cause mix-ups. Even with electronic systems, if the prescriber selects the wrong strength or the pharmacy tech doesn’t double-check, the error slips through. Then there’s dispensing errors, when the right drug is given but in the wrong form, quantity, or instructions. Think giving a 30-day supply of insulin instead of 10, or labeling a child’s antibiotic with adult dosing. These aren’t theoretical—they’ve led to hospitalizations and deaths.
It’s not just about the pills. pharmacy safety, the system of checks, training, and communication that protects patients from harm often breaks down when staff are overworked. A pharmacist juggling 100 prescriptions in a shift won’t catch every interaction. A tech rushing to meet quotas might skip verifying allergies. And patients? They rarely ask questions. They assume the pharmacist knows what they’re doing. But if you’re on five medications, have kidney issues, or take supplements, you need to speak up. The system isn’t perfect. Your vigilance matters.
Some mistakes are hidden. Like when a pharmacy substitutes a generic without checking if it’s safe for a narrow therapeutic index drug—like warfarin or levothyroxine. Or when they don’t flag that a new antibiotic could cancel out your birth control. Or when they fail to offer large-print labels to someone with low vision. These aren’t big scandals. They’re quiet failures that pile up. And they’re preventable.
Below, you’ll find real cases and clear breakdowns of what goes wrong in everyday pharmacy settings. From how EHR integration can reduce errors to why pediatric dosing mistakes still happen, these posts show you the gaps—and how to protect yourself. You’ll learn what to watch for when picking up your prescription, how to question a label, and which red flags mean you should walk back to the counter. This isn’t about blaming pharmacists. It’s about understanding where the system is weak so you can fill the gaps before it’s too late.
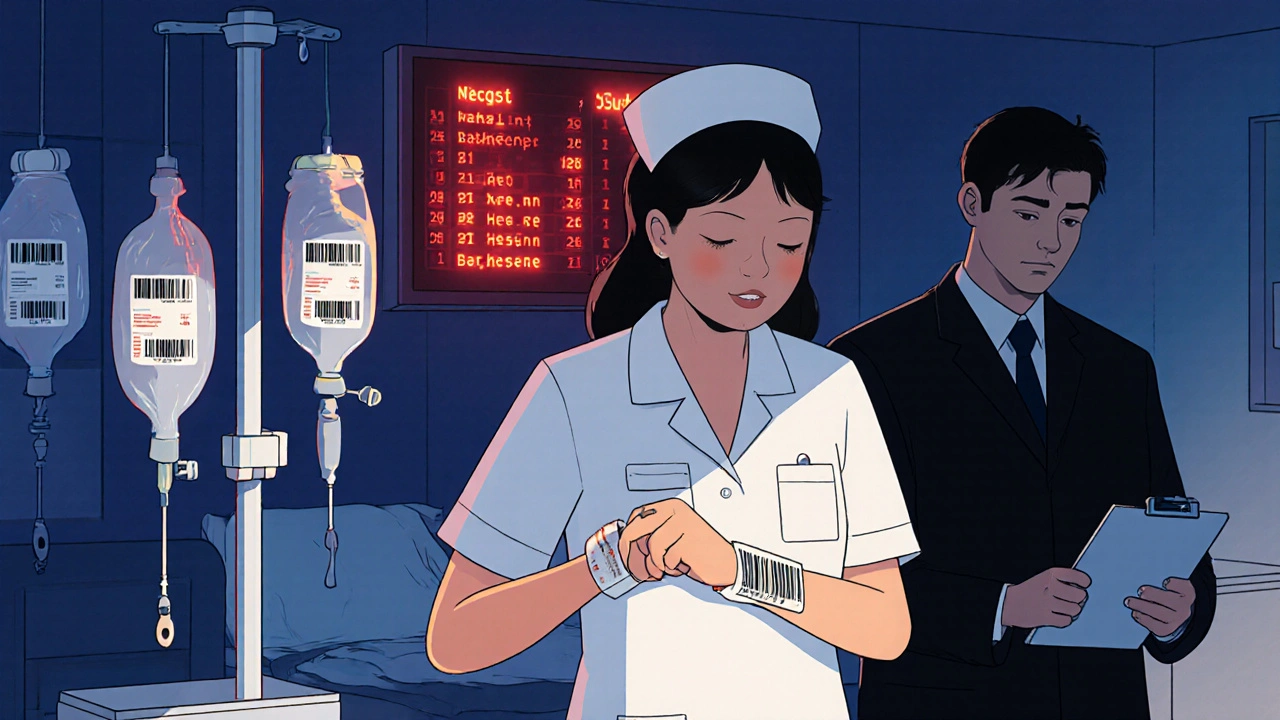
Medication errors are common in both hospitals and retail pharmacies, but the types, causes, and consequences differ. Learn how errors happen in each setting and what you can do to protect yourself.
View more