When you hear transdermal fentanyl, a long-acting opioid pain medication delivered through a skin patch. Also known as fentanyl patch, it's not your average pain reliever—it's designed for people with severe, ongoing pain who need steady relief around the clock. Unlike pills that spike and drop in your system, this patch slowly releases fentanyl through your skin over 72 hours. That’s why doctors prescribe it for cancer pain, severe arthritis, or other chronic conditions where daily opioids aren’t enough—or too risky to take repeatedly.
But here’s the catch: fentanyl patches, a controlled opioid delivery system used in chronic pain management aren’t for beginners. They’re not for occasional pain, not for post-surgery use, and definitely not for someone who’s never taken opioids before. The dose is intense—a single patch can contain enough fentanyl to kill someone who isn’t tolerant. That’s why misuse, accidental exposure (like a child finding a used patch), or improper application can be deadly. The FDA has issued multiple warnings about this, and emergency rooms see cases every year from people who didn’t realize how powerful it is.
That’s where chronic pain management, a structured approach to treating persistent pain with medication, therapy, and lifestyle changes comes in. Transdermal fentanyl isn’t a standalone fix. It’s one tool in a bigger plan that includes physical therapy, non-opioid meds, and regular check-ins with your doctor. Many patients on these patches also take other drugs for side effects—like nausea or constipation—which is why knowing how opioids interact with other medications matters. For example, mixing fentanyl with certain sleep aids or anxiety meds can slow your breathing to dangerous levels.
And it’s not just about the drug itself—it’s about how it’s used. People often leave patches on too long, cut them to stretch the dose, or apply them to warm skin (like near a heating pad), which speeds up absorption and can cause overdose. Even storing them improperly—like in a pocket or drawer where kids or pets can reach them—is a real danger. The patch isn’t just medicine; it’s a controlled substance that needs the same care as a loaded gun.
There are alternatives, too. Some patients switch to extended-release oral opioids, others try non-opioid nerve pain drugs like gabapentin, or even non-drug options like spinal cord stimulators. But for those who’ve tried everything else and still can’t function without relief, transdermal fentanyl remains a critical option—if used correctly.
In the posts below, you’ll find real-world advice on how these patches are prescribed, how to avoid common mistakes, what side effects to watch for, and how patients manage life while using them. You’ll also see how cost, access, and generic alternatives play into the bigger picture of opioid therapy. Whether you’re a patient, caregiver, or just trying to understand why this patch is so talked about, the information here is practical, no-fluff, and focused on what actually matters for safety and effectiveness.
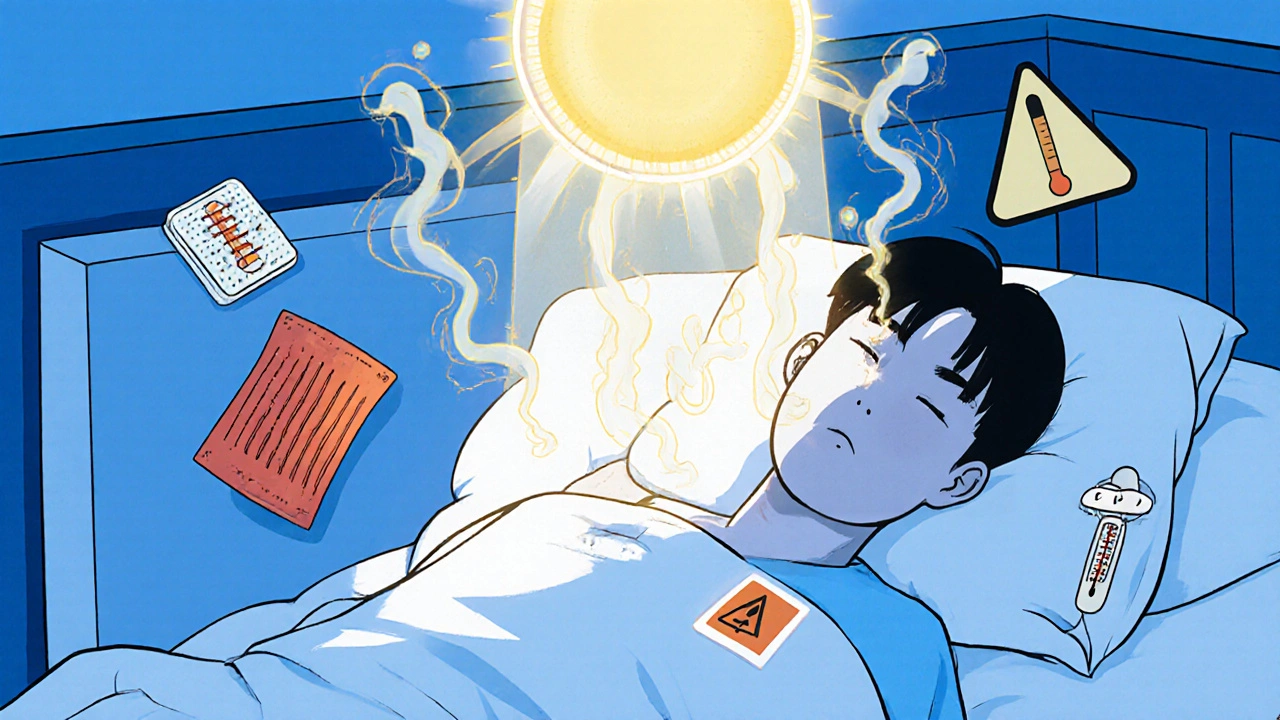
Fentanyl patches can be life-saving for chronic pain - but heat from showers, fever, or heating pads can cause deadly overdose. Learn what really increases absorption and how to stay safe.
View more