When you hear trastuzumab, a monoclonal antibody used to treat certain types of breast cancer. Also known as Herceptin, it doesn't work like traditional chemo—it targets cancer cells directly, sparing healthy tissue where it can. This isn't a one-size-fits-all drug. It only helps people whose cancer tests positive for HER2, a protein that fuels aggressive tumor growth. About 1 in 5 breast cancers are HER2-positive, and for those patients, trastuzumab changed everything—turning a once-deadly diagnosis into a manageable condition for many.
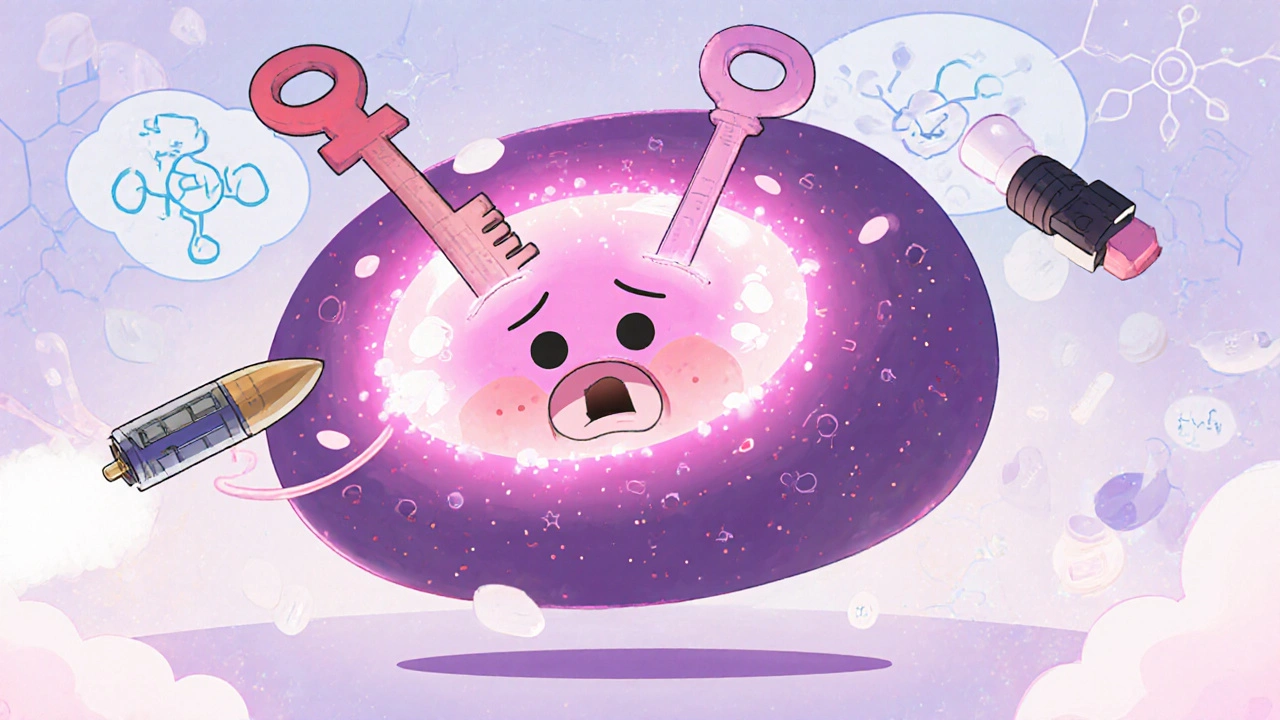
Trastuzumab works by latching onto HER2 receptors on cancer cells like a key in a lock. Once attached, it blocks signals telling the cell to multiply and flags the cell for destruction by the immune system. It’s often used with chemo at first, then sometimes alone for maintenance. But it’s not just about the drug itself—it’s about how it fits into a bigger picture. HER2-positive breast cancer, a subtype of breast cancer driven by overexpression of the HER2 protein requires different monitoring than other types. Doctors track heart function closely because trastuzumab can weaken the heart in some people. That’s why regular echocardiograms are part of the treatment plan. And while it’s not a cure for everyone, it’s often the difference between survival and progression.
It’s also part of a growing trend in cancer care: targeted therapy, treatments designed to attack specific molecular features of cancer cells. Unlike chemo, which hits all fast-growing cells, targeted drugs like trastuzumab are precise. That means fewer side effects like hair loss or severe nausea—but not zero. Fatigue, fever, and chills are common, especially during the first infusion. Some patients worry about long-term heart damage, but studies show that with careful monitoring, most people tolerate it well. And when combined with newer drugs like pertuzumab or T-DM1, outcomes improve even more.
Trastuzumab isn’t just for breast cancer. It’s also used in some cases of advanced stomach cancer with HER2 overexpression. The same principle applies: test for the marker, then treat accordingly. This is personalized medicine in action—not guessing, but knowing. And that’s why the posts below cover real-world concerns: how to manage side effects, what to expect during infusions, how insurance handles these expensive drugs, and why generic versions are starting to appear. You’ll find guides on treatment timelines, patient stories, and how to talk to your oncologist about options. This isn’t theoretical. It’s what people are living through every day.
HER2-positive breast cancer, once aggressive and hard to treat, now has multiple targeted therapies that improve survival and quality of life. Learn how trastuzumab, T-DXd, tucatinib, and other drugs work, their side effects, and what’s next in treatment.
View more