When we talk about drug safety, the practices and systems designed to prevent harm from medications. Also known as medication safety, it’s not just about reading the label—it’s about knowing when a pill can turn dangerous because of heat, age, weight, or even what else you’re taking. Every year, thousands of people end up in emergency rooms not because they took too much, but because they didn’t understand how their medication behaved under certain conditions.
Opioid safety, the set of precautions needed to prevent overdose and misuse of pain medications, is one of the most urgent areas of drug safety today. Fentanyl patches, for example, can be life-saving for chronic pain—but if you take a hot shower or use a heating pad, your body absorbs the drug too fast. That’s not a side effect. That’s a silent killer. And it’s not just opioids. Pediatric drug safety, the careful calculation and administration of medicines for children based on weight and development is just as critical. A simple dosing mistake in mg/kg can turn a helpful treatment into a life-threatening error. Kids aren’t small adults. Their bodies process drugs differently, and wrong numbers don’t just cause nausea—they can stop breathing.
Then there’s the quiet side of drug safety: how generics are tested and trusted. Therapeutic equivalence, the standard that ensures generic drugs perform the same way as brand-name versions is the backbone of affordable care. But it’s not foolproof. Some combination pills, like those for high blood pressure or epilepsy, have narrow therapeutic windows. Even tiny differences in inactive ingredients can throw off how the drug works. The FDA’s Orange Book helps, but it’s not a guarantee. You still need to watch for changes in how you feel after a switch.
And it’s not just about the medicine itself. It’s about who’s taking it. Pregnant women weighing antidepressant risks. Older adults juggling five prescriptions that interact in ways no doctor fully predicts. People with low vision struggling to read tiny print on labels. These aren’t edge cases—they’re everyday realities. Drug safety doesn’t end at the pharmacy counter. It starts with awareness, continues with communication, and ends with action.
Below, you’ll find real, practical guides on exactly how these risks show up—and how to avoid them. From how heat turns fentanyl patches into traps, to why some generics are safer than others, to how to calculate a child’s dose without guessing. No theory. No fluff. Just what works.
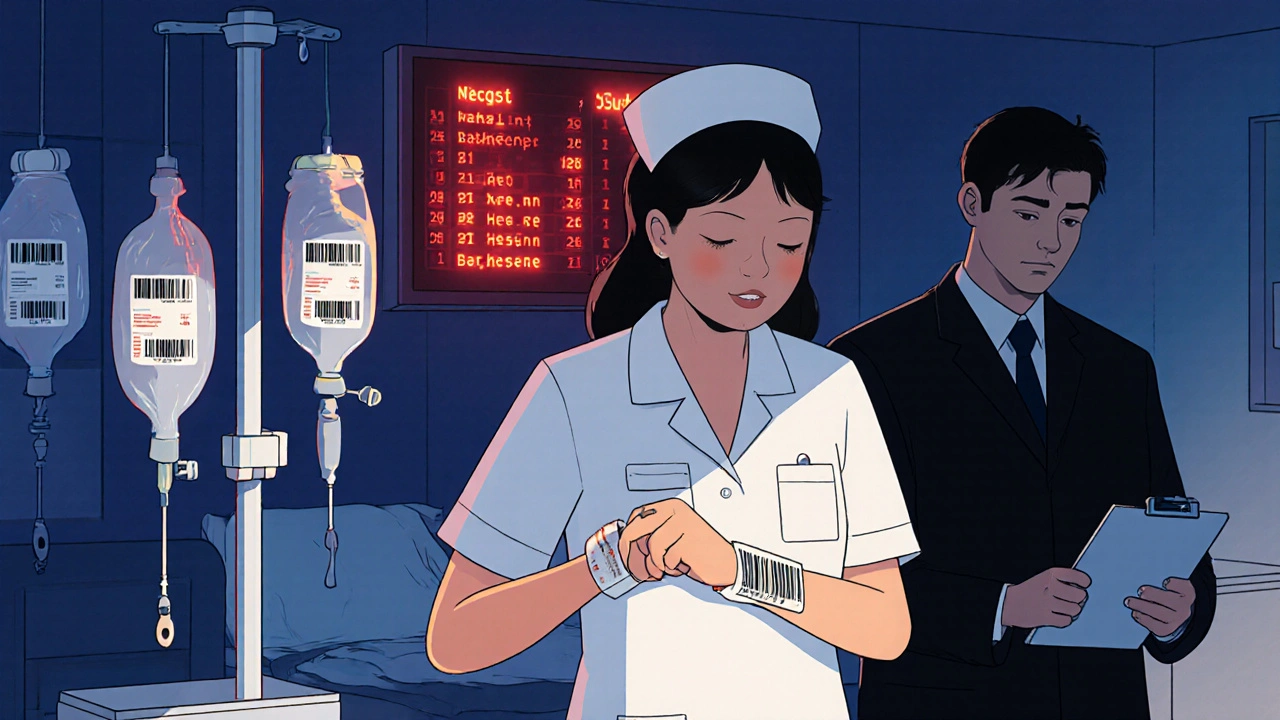
Medication errors are common in both hospitals and retail pharmacies, but the types, causes, and consequences differ. Learn how errors happen in each setting and what you can do to protect yourself.
View more