When you hear generic drugs, medications that contain the same active ingredients as brand-name drugs but are sold without a brand name. Also known as non-brand medications, they are the backbone of affordable healthcare worldwide. They aren’t cheaper because they’re weaker—they’re cheaper because they don’t carry the marketing, advertising, or patent costs of the original. The FDA requires them to work the same way, in the same amount, and with the same safety profile. But not all generics are created equal, and knowing the difference can save you money—or even your life.
One key type is the authorized generic, a version made by the original brand-name company and sold under a different label. These are identical to the brand in every way, down to the inactive ingredients. If you’re switching from a high-cost brand like Lipitor or Advair, an authorized generic gives you the exact same result without the price tag. Then there’s therapeutic equivalence, the official rating that says one generic can safely replace another. But here’s the catch: for drugs with a narrow therapeutic index—like warfarin, levothyroxine, or epilepsy meds—even small differences in absorption can cause serious problems. That’s why some doctors and pharmacists are cautious, even when the label says "equivalent".
Big savings come from bulk purchasing generics, when clinics, pharmacies, or hospitals buy large quantities to get deep discounts. Some providers cut drug costs by over 20% this way, using secondary distributors or stock nearing expiration (but still safe). It’s how low-income countries get life-saving HIV or diabetes meds at 80% less than U.S. prices. But it’s not just about volume—it’s about knowing which generics to trust. Some are made in the same factories as the brand, others in plants with less oversight. And heat? That’s another hidden risk. Fentanyl patches, for example, can overdose you if you’re in a hot shower or feverish—even if you’ve been stable for months.
Switching to generics isn’t just a cost move—it’s a strategy. Whether you’re managing chronic pain, depression, or high blood pressure, the right generic can work just as well. But you need to ask questions: Is this an authorized generic? Does my condition need extra care? Am I getting the same formulation? And if you’re buying in bulk, are you sure the supply chain is reliable? The posts below break down exactly how to navigate these choices safely—whether you’re a patient, caregiver, or provider. You’ll find real-world advice on switching medications, avoiding errors, understanding dosing, and spotting the hidden risks that most people never hear about.
Batch-to-batch variability can skew bioequivalence results, leading to false approvals or rejections of generic drugs. Learn how regulators are updating standards to account for real-world manufacturing differences.
View more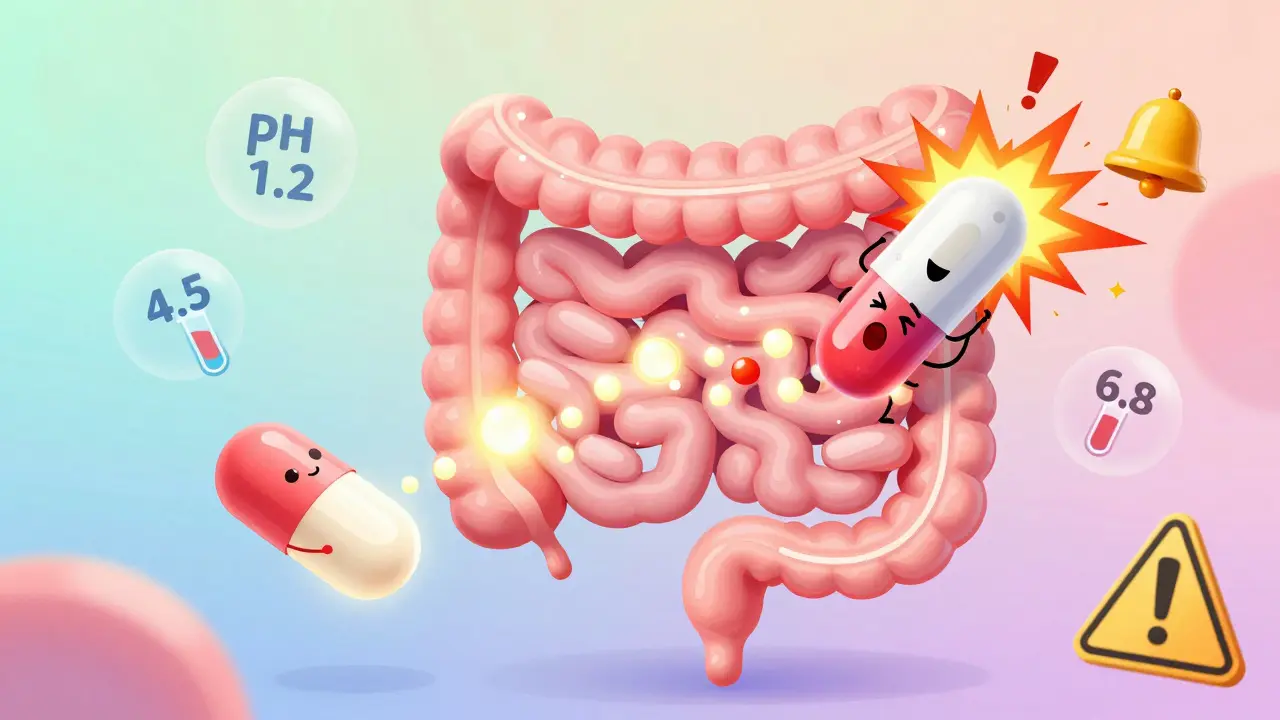
Modified-release formulations require special bioequivalence testing to ensure generic versions match the brand's release pattern. Learn the key rules, regulatory differences, and why many generics fail.
View more
Understanding how generic drugs degrade over time and why shelf life matters for safety. Learn the science behind stability testing, risks of expired medications, and how storage impacts effectiveness.
View more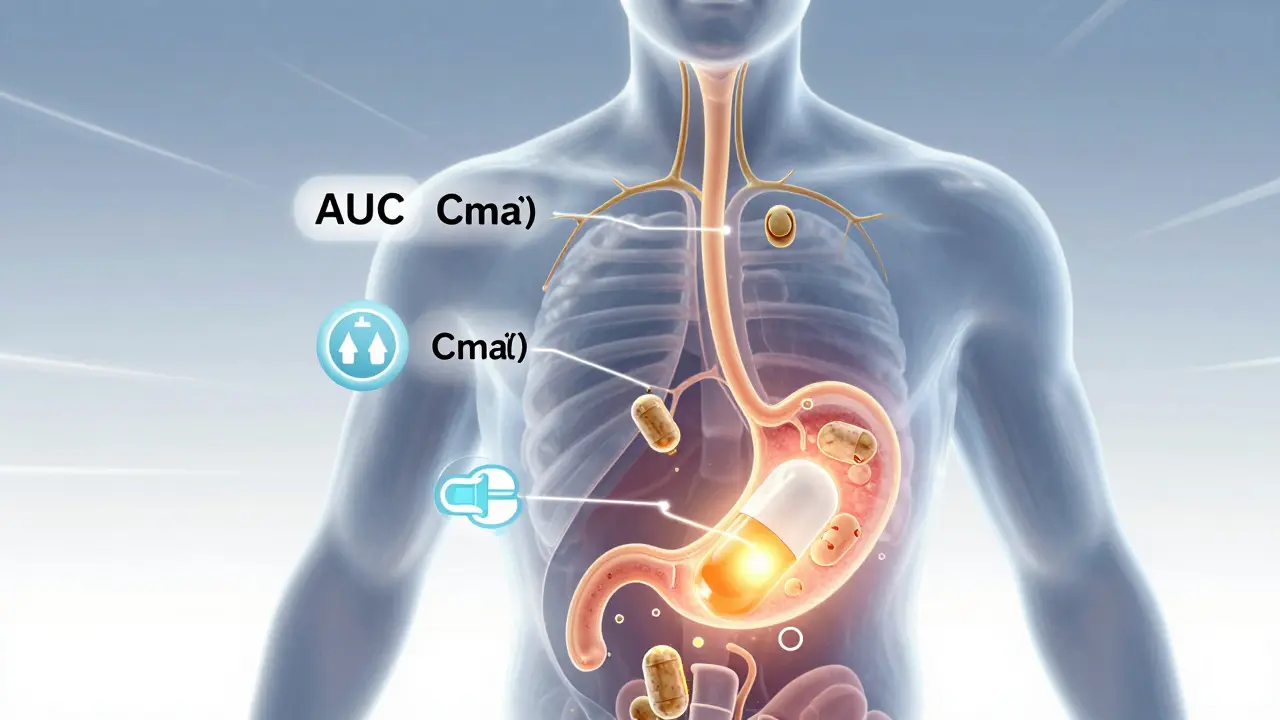
Bioavailability studies ensure generic drugs are absorbed the same way as brand-name versions. The FDA uses precise pharmacokinetic tests to confirm safety and effectiveness before approval.
View more
Many people feel generic medications don’t work as well as brand-name drugs - but the difference is often psychological, not chemical. Learn how expectations shape treatment outcomes and what you can do about it.
View more
Not all drugs have authorized generics - and when they do, it's often a strategic move by brand manufacturers to control pricing. Learn why some drugs have them, others don't, and what it means for your prescription costs.
View more
Bioequivalence testing for combination products-like fixed-dose pills, topical creams, and inhalers-is far more complex than for single-drug generics. Learn why these products face higher failure rates, higher costs, and regulatory hurdles that delay affordable access.
View more
Therapeutic equivalence ensures generic drugs work just like brand-name ones, keeping patients safe while cutting costs. Learn how the FDA's Orange Book system protects you and why it matters for your treatment.
View more